To the Editor:
Gaucher disease, the inherited deficiency of lysosomal glucocerebrosidase, is currently managed with enzyme replacement therapy using a mannose-terminated form of human glucocerebrosidase.1 This therapy, costing $100,000 to $400,000 per adult per year, effectively improves the biochemical and hematologic manifestations of the disorder and reverses hepatosplenomegaly in most patients.1-4 We describe an Ashkenazi patient with type 1 Gaucher disease demonstrating massive hepatosplenomegaly, anemia, and thrombocytopenia, who, despite 2 years of aggressive high-dose enzyme replacement therapy, ultimately required a splenectomy for effective management.
The patient, diagnosed with Gaucher disease at 36 years of age, presented with anemia and an abdominal mass; a bone marrow biopsy showed Gaucher cells. Examination at 41 years of age showed a markedly protuberant abdomen with a massive spleen, brimming over the pelvis; the hemoglobin level was 7.3 g/dL, the hematocrit level was 23.6, and there were 22,000 platelets/μL. Acid phosphatase, ferritin, angiotensin-converting enzyme, and IgM levels were elevated. His genotype was N370S/N370S. Skeletal involvement was minimal. Using magnetic resonance imaging (MRI), his splenic volume was 9,130 mL and his hepatic volume was 3,600 mL.
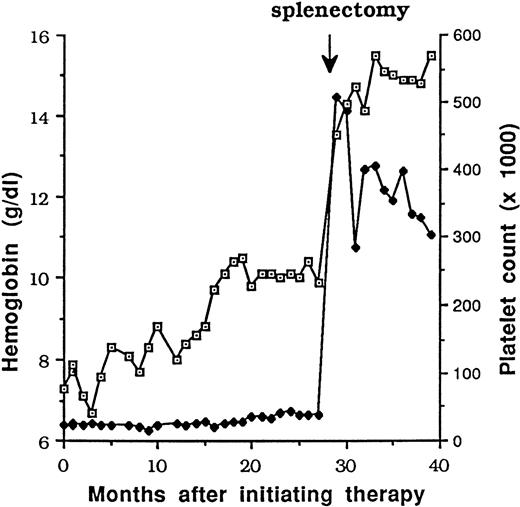
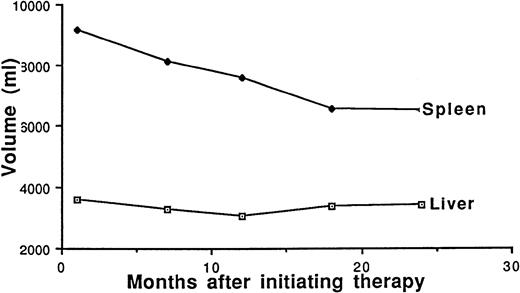
Alglucerase was administered at 120 IU/kg/mo, resulting initially in a slow but gradual increase in hemoglobin level and a decrease in spleen size, although his thrombocytopenia was unaltered (Fig 1A and B). After 18 months of therapy, his initial response plateaued, and a splenectomy was performed.
Response to therapy over time. (A) Response of (⊡) hemoglobin (in grams per deciliter) and (⧫) platelets after initiation of therapy. (B) (⊡) Hepatic and (⧫) splenic volumes.
Response to therapy over time. (A) Response of (⊡) hemoglobin (in grams per deciliter) and (⧫) platelets after initiation of therapy. (B) (⊡) Hepatic and (⧫) splenic volumes.
After surgery, his counts stabilized and remained in the high normal range, and other laboratory parameters were corrected. Enzyme replacement was resumed at a reduced dose.
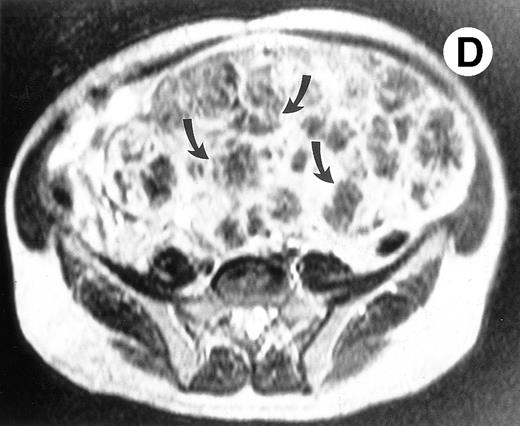
Surgical pathology showed a 6.5-kg spleen with nodular appearing external surfaces and focal subcapsular infarcts, ranging in size from 0.5 to 3.4 cm. Serial sections showed rubbery and focally fibrotic surfaces (Fig 2A). This correlated with his presurgical axial T2-weighted MRI, which demonstrated multiple low signal intensity nodules not seen on T1-weighted views (Fig 2B through D). Although MRI is useful in monitoring response to therapy, this case demonstrates that volumetric measurements alone may not be adequate, especially when there are multiple areas of decreased signal intensity on T2-weighted STIR images. Both splenic nodules and infarcts are common in Gaucher patients, occuring in approximately 30% and 32% of patients, respectively.5 Thus, the volume free of nodules and infarct may be a more reliable measure of response to enzyme therapy in these patients.
(A) Photograph of the patient's spleen showing multiple nodules (arrows) with area of subcapsular infarcts (curved arrows). (B) Coronal STIR MR image of the (L) liver and spleen (IR 2450/100/30) shows multiple low signal intensities nodules (curved arrows) in the enlarged spleen. (C) Axial T1-weighted (SE 300/10) MR image shows splenomegaly with no focal splenic signal abnormality. (D) Axial T2-weighted (SE 4293/80) MR image of the spleen at the same level as (C) shows multiple low signal intensity nodules in the enlarged spleen (arrows).
(A) Photograph of the patient's spleen showing multiple nodules (arrows) with area of subcapsular infarcts (curved arrows). (B) Coronal STIR MR image of the (L) liver and spleen (IR 2450/100/30) shows multiple low signal intensities nodules (curved arrows) in the enlarged spleen. (C) Axial T1-weighted (SE 300/10) MR image shows splenomegaly with no focal splenic signal abnormality. (D) Axial T2-weighted (SE 4293/80) MR image of the spleen at the same level as (C) shows multiple low signal intensity nodules in the enlarged spleen (arrows).
This patient's suboptimal response to high-dose Alglucerase therapy is likely due to the massive load of stored lipid, which accumulated before therapy, both in focal nodules and individual cells. The hematologic sequelae of massive splenic enlargement often necessitates clinical intervention. Generally, with rare exceptions,1,3,4 enzyme replacement therapy will decrease splenic volume by 50% to 75% over 2 years.1-3 The majority of this patient's spleen, with its marked nodularity and fibrosis, did not appear to be accessible to the infused enzyme, which may not easily debulk organs with massive storage.
Enzyme replacement therapy can effectively improve the multisystem involvement seen among patients with Gaucher disease. Because medical therapy is now available, the appropriate criteria for splenectomy must be reconsidered. Although the medical consequences of delaying splenectomy in this case may have been minimal, the economic burden (>$800,000 for this patient) cannot be easily overlooked. A suboptimal hematologic response to an adequate trial of enzyme replacement is an appropriate indication for splenectomy. The prohibitive cost of enzyme may be sufficient criteria in certain circumstances. A T2-weighted MRI showing an enlarged spleen with multiple hypodense nodules may indicate that large damaged regions are inaccessible to infused enzyme, necessitating splenectomy. Other emergencies, including the need for rapid surgical correction of thrombocytopenia, an inferior vena cava syndrome, severe abdominal pain crises, and splenic abscesses, continue to be valid rationale. The question of whether, in similar patients with massive organomegaly, splenic nodules, and thrombocytopenia, splenectomy should be the initial therapy, remains to be determined.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal