Abstract
Marginal zone cell lymphoma is a recently described entity among the non-Hodgkin's lymphomas. It likely originates from the marginal zone B cells in the spleen and equivalent cells in the lymph node and extranodal tissues. Recent evidence indicates that marginal zone B cells are functionally heterogeneous and may differ with respect to the pattern of somatic hypermutation in their Ig variable genes. To test whether marginal zone lymphomas may originate from different subsets of marginal zone B cells, we performed a sequence and mutation analysis of the rearranged Ig heavy chain (IgH) variable genes (Vh) of a series of 14 cases of marginal zone lymphoma, occurring in the spleen (4), the lymph node (4), the stomach (2), the orbit (2), the tongue (1), and the skin (1). Our data show that marginal zone cell lymphomas preferentially rearrange the Vh4, Vh3, and Vh1 family genes, without preference for any particular Vh gene. Somatic mutations are present in 13 cases; one case of marginal zone cell lymphoma of the skin showed a germline configuration of the rearranged Vh gene. Mutation analysis shows evidence of antigen selection in three cases of marginal zone cell lymphoma, one of the spleen, stomach, and orbit, respectively. No evidence of antigen selection was present in the other cases. These data indicate that marginal zone cell lymphomas may arise from different subsets of marginal zone B cells. In addition, lymphomagenesis may not be triggered by antigen in all cases of marginal zone cell lymphoma.
MARGINAL ZONE cell lymphoma is a recently recognized entity among the non-Hodgkin's lymphomas.1 It typically occurs in the spleen.2,3 Although clinically distinct, the monocytoid B-cell lymphomas of the lymph node and the lymphomas of the extranodal sites, the so-called MALT lymphomas, have also been argued to represent marginal zone cell lymphomas based on similar morphological, immunophenotypic and cytogenetic features.4-6 The lymphoma cells characteristically express pan B-cell markers such as CD20 and CD22 but no CD5, CD10, or CD23. IgM, or to a lesser extent IgA or IgG are expressed. IgD is variably coexpressed.7-9 Trisomy 3 is the most frequently detected cytogenetic abnormality in marginal zone cell lymphomas.10,11 Because of the localization, morphology, and immunophenotypic characteristics, marginal zone cell lymphomas are thought to derive from marginal zone cells of the spleen or equivalent cells in the lymph nodes and extranodal tissues. Interestingly, normal marginal zone B cells are most likely a functionally heterogeneous population of B cells.12 From studies in rodents, it is clear that the marginal zone contains three distinct subsets of B cells. Two subsets represent memory B cells generated by a T-cell–dependent (TD) and T-cell–independent type 1 (TI-1) immune reaction, respectively. The third population of marginal zone cells do not represent memory cells and are involved in the T-cell–independent primary immune reaction to type 2 antigens (TI-2).12Mutation analysis of rearranged Vh genes of human microdissected marginal zone B cells provided evidence that human marginal zone B cells may be functionally heterogeneous as well.13,14 Only a subpopulation of the cells shows a characteristic pattern of somatic mutations in the rearranged Vh genes indicative of positive antigen selection or affinity maturation and therefore likely participates in the T-cell–dependent immune reaction. The rearranged Vh genes of the other marginal zone B-cell subset show somatic mutations that do not exhibit the distribution pattern characteristic of affinity maturation. It was postulated that this subset of marginal B cells is an early memory B cell of the TD immune reaction.13 The relative presence of these subsets of B cells probably differs between the marginal zones in the spleen and Peyer's patch,14 attributed to the differences in antigen exposure in these organs.14 In addition, circumstantial evidence shows that a subset of human splenic marginal zone cells is involved in the TI immune response.15 The presence of somatic mutations in these cells is not yet documented.
The presence of distinct B-cell subsets in the marginal zone led us to postulate that the marginal zone cell lymphomas arise from different subsets of marginal zone cells. To test this hypothesis, we performed a Vh gene mutation analysis of a series of marginal zone cell lymphomas.
MATERIALS AND METHODS
Case selection.
We selected 14 cases of marginal zone cell lymphoma documented by morphology and immunophenotypic analysis. Four patients presented with primary lymphoma in the spleen, four in the lymph node, two in the gut, two in the orbit, one in the skin, and one in the tongue. Most of the patients were included in a previous study.11 The patient and lymphoma characteristics are summarized in Table1. In addition, cyclin D1 staining was performed in case 13, to rule out the possibility of a diagnosis of mantle cell lymphoma. Two monoclonal anti-cyclin D1 antibodies (Novocastra, Newcastle upon Tyne, UK; Immuno-Biological Laboratories, Gunma, Japan) were used, but no cyclin D1 was expressed by the lymphoma cells. The clinical history of a lymphoma that has been recurring at the same site for 7 years without dissemination to other locations strongly argues against the diagnosis of mantle cell lymphoma as well.
Characteristics of the Marginal Zone Lymphomas
| Case . | Site of Primary Involvement . | Age/Sex . | Immunophenotype . | |||||
|---|---|---|---|---|---|---|---|---|
| CD20 . | CD5 . | IgM . | IgD . | κ . | λ . | |||
| 1 | Spleen | 65/M | + | − | + | − | + | − |
| 2 | Spleen | 71/M | + | − | + | − | + | − |
| 3 | Spleen | 52/M | + | − | + | − | + | − |
| 4 | Spleen | 69/M | + | − | + | +/− | − | + |
| 5 | Lymph node | 84/M | + | − | +/− | − | − | + |
| 6 | Lymph node | 55/F | + | − | +/− | − | − | + |
| 7 | Lymph node | 65/M | + | − | + | − | + | − |
| 8 | Lymph node | 59/M | + | − | + | − | + | − |
| 9 | Stomach | 68/F | + | − | + | − | + | − |
| 10 | Stomach | 56/F | + | − | + | − | + | − |
| 11 | Orbit | 57/M | + | − | + | − | − | + |
| 12 | Orbit | 71/F | + | − | + | − | + | − |
| 13 | Skin | 60/M | + | − | + | + | − | + |
| 14 | Tongue | 59/M | + | − | + | +/− | + | − |
| Case . | Site of Primary Involvement . | Age/Sex . | Immunophenotype . | |||||
|---|---|---|---|---|---|---|---|---|
| CD20 . | CD5 . | IgM . | IgD . | κ . | λ . | |||
| 1 | Spleen | 65/M | + | − | + | − | + | − |
| 2 | Spleen | 71/M | + | − | + | − | + | − |
| 3 | Spleen | 52/M | + | − | + | − | + | − |
| 4 | Spleen | 69/M | + | − | + | +/− | − | + |
| 5 | Lymph node | 84/M | + | − | +/− | − | − | + |
| 6 | Lymph node | 55/F | + | − | +/− | − | − | + |
| 7 | Lymph node | 65/M | + | − | + | − | + | − |
| 8 | Lymph node | 59/M | + | − | + | − | + | − |
| 9 | Stomach | 68/F | + | − | + | − | + | − |
| 10 | Stomach | 56/F | + | − | + | − | + | − |
| 11 | Orbit | 57/M | + | − | + | − | − | + |
| 12 | Orbit | 71/F | + | − | + | − | + | − |
| 13 | Skin | 60/M | + | − | + | + | − | + |
| 14 | Tongue | 59/M | + | − | + | +/− | + | − |
cDNA synthesis.
RNA was extracted from 10 20-μm frozen tissue sections using TRIzol reagent (Life Technologies, Gaithersburg, MD) following the manufacturer's recommendations. In this study, 1 μg of total RNA was used for reverse transcription (RT). RT was performed using Superscript II Reverse Transcriptase (Life Technologies) according to the manufacturer's instructions. Briefly, the RNA was added to 8 μL DEPC-treated H2O containing 150-ng random primers (Life Technologies). This mixture was heated to 70°C for 10 minutes and quickly chilled on ice water. Subsequently, 12 μL of a reaction mixture containing 15 mmol/L KCl, 10 mmol/L Tris–HCl, pH 8.3, 0.75 mmol/L MgCl2, 0.1 mol/L DTT, 10 mmol/L dNTPs, 200 U Reverse Transcriptase and 2.5 U Ribonuclease Inhibitor (Life Technologies) was added.
PCR amplification of the rearranged Ig heavy chain genes.
A total of 4 μL of a 1:100 dilution of the cDNA product was used for the polymerase chain reaction (PCR). The rearranged Ig heavy chain genes were amplified using a semi-nested PCR method as previously described.16 In the first round of the PCR, a mixture of six framework I (FR I) Vh family-specific primers and three primers complementary to all Jh genes was used. The second round of the PCR was performed in six separate reactions with one of the six Vh FR I primers and internal Jh primers.
The DNA was added to the PCR buffer (50 mmol/L KCl, 10 mmol/L Tris–HCl pH 8.4, 0.01% gelatin) containing 200 μmol/L dNTPs, 2.5 mmol/L MgCl2, 100 nmol/L of each primer, and 1.5 U Taq polymerase, in a total volume of 50 μL. In the second round of amplification, the same reagent concentrations were used, except for that of MgCl2, which was 1.5 mmol/L; 2 μL of the first-round PCR product was added to the semi-nested reaction as the template. The PCR conditions of the first round consisted of one cycle at 95°C for 2 minutes, 59°C for 4 minutes, 72°C for 80 seconds followed by 34 cycles at 95°C for 90 seconds, 59°C for 30 seconds, 72°C for 80 seconds, and one final cycle of 72°C for 5 minutes. The second PCR consisted of a total of 35 cycles, using annealing temperatures of 65°C and 61°C for the Vh3, Vh4, and Vh1, Vh2, Vh5, Vh6, primers, respectively. The denaturing and extension temperatures as well as the cycle conditions were identical to those of the first round of PCR. All PCR reactions were performed using a hot-start procedure and appropriate positive and negative controls. All samples were analyzed in duplicate. An aliquot of 10 μL PCR product was size-fractionated through a 6% polyacrylamide gel (PAGE) in 1× TBE buffer.
Sequencing of the PCR products.
The PCR products to be sequenced were gel-purified. Briefly, the gel bands containing the monoclonal rearranged VH gene PCR products were excised from the 6% PAGE and eluted in TE buffer (50 mmol/L Tris, 1 mmol/L EDTA; pH 7.4) at 55°C. Two microliters of this PCR product was re-amplified in a 50-μL volume using the respective VH family-specific primer and the internal JH primers as in the second PCR amplification. Forty microliters of re-amplified PCR products were subsequently analyzed on a 1.5% agarose gel. The appropriate bands were excised and the PCR products were extracted from the gel with Qiaquick spin columns (Qiagen GmbH, Hilden, Germany) following the manufacturer's recommendations.
An aliquot of the isolated DNA was directly sequenced on both strands, using Sanger's chain termination method and fluorescent dideoxynucleotide chain terminators.17 Sequencing primers were identical to the primers used for the second round of the semi-nested PCR of the rearranged Vh genes. The Jh primer used for the reverse sequencing reaction was determined based on the sequence obtained in the forward sequencing reaction. The products of the sequencing reaction were analyzed using the Applied Biosystems 373A sequenator (Applied Biosystems, Foster City, CA).
Sequence analysis.
The identification of the Vh, Ig heavy chain diversity genes (Dh) and Jh germline sequences was performed by sequence comparison to the March 1997 update of V Base, a comprehensive database of human Ig germline gene sequences compiled from published sequences (V BASE sequence directory, I.M. Tomlinson, MRC Centre for Protein Engineering, Cambridge, UK). Mac Vector 5.0 sequence analysis software (Oxford Molecular Group, Campbell, CA) was used for this sequence analysis. For the germline DH gene attribution, the longest stretches with the highest homology were retained with a minimum of six successive matches or seven successive matches, interrupted by one mismatch.
Somatic mutation analysis.
The probability that somatic mutations in the rearranged Vh genes resulted from antigen selection was analyzed according to Chang and Casali.18 The probability that an excess of replacement (R) mutations in Vh complementarity determining regions (CDRs) or FRs occurred on the basis of chance alone was calculated using the binomial distribution model
wheren is the total number of observed mutations, k is the number of observed R mutations in the CDRs or the FRs, and q is the probability that an R mutation will localize to CDRs or FRs:
The inherent susceptibility of R mutations of the CDRs and FRs (CDR Rf and FR Rf, respectively) has been calculated for each of the identified germline genes and is based on the chances of the occurrence in each codon of an amino acid replacement, given any single nucleotide change that does not result in a termination codon.
RESULTS
Sequence analysis.
The distribution of the Vh gene families used by the marginal zone cell lymphoma cases studied is summarized in Table2. The marginal zone cell lymphoma cases preferentially rearranged gene members of the Vh4 family and, to a lesser extent, of the Vh3 and Vh1 families. The nucleic acid sequences are available from Genbank. The deduced amino acid sequences are given in Fig 1. No preferential rearrangement involving any particular Vh gene was seen. A slight overrepresentation of the Dh gene family Dxp was observed in the lymph node- and spleen-based marginal zone cell lymphomas. In four of six cases of MALT lymphomas no definitive assignment of the Dh gene could be made. In case 14, a Dh gene was absent. A predominance of JH4 and JH6 gene rearrangements was observed.
Mutation Analysis of the Marginal Zone Lymphomas
| Case . | Sequence . | Germline VH Gene (reference) . | % Identity . | N . | Obs R/S . | Exp R CDR . | Exp R FR . | p CDR . | p FR . | Germline DH Gene . | Germline JH Gene . | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CDR . | FR . | |||||||||||
| 1 | VH4 | DP 79* | 97.70 | 5 | 2/0 | 1/2 | 1.3 | 2.6 | .273 | .134 | Dxp′1 | JH4 |
| 2 | VH4 | DP 71 (42) | 93.10 | 15 | 0/2 | 3/10 | 3.6 | 7.9 | .018 | .007 | D1 | JH4 |
| 3 | VH1 | DP 25 (42) | 96.40 | 8 | 4/0 | 3/1 | 1.9 | 4.4 | .075 | .075 | Dxp′1 | JH6 |
| 4 | VH3 | DP 77* | 97.80 | 6 | 1/2 | 2/1 | 2.7 | 1.2 | .401 | .401 | DN1 | JH5 |
| 5 | VH4 | DP 66 (42) | 93.20 | 9 | 0/3 | 4/2 | 2.1 | 5.2 | .073 | .234 | Dxp 4 | JH6 |
| 6 | VH4 | DP 65 (42) | 92.70 | 19 | 2/2 | 8/7 | 4.9 | 9.3 | .100 | .154 | Dxp 1/D21/Dxp 4 | JH6 |
| 7 | VH4 | DP 63 (42) | 97.30 | 6 | 2/0 | 2/2 | 1.5 | 3.2 | .299 | .203 | NI | JH6 |
| 8 | VH1 | DP 10 (42) | 96.50 | 8 | 1/2 | 1/4 | 1.9 | 4.4 | .276 | .276 | D21-9/D21-7 | JH6 |
| 9 | VH3 | V4-34 (43) | 96.76 | 7 | 4/0 | 1/2 | 1.8 | 3.6 | .060 | .047 | NI | JH4 |
| 10 | VH4 | DP 49 (44) | 96.80 | 7 | 2/1 | 3/1 | 1.7 | 3.8 | .310 | .240 | NI | JH4 |
| 11 | VH3 | COS 16* | 92.44 | 17 | 9/0 | 5/3 | 3.9 | 9.3 | .006 | .031 | NI | JH4 |
| 12 | VH4 | DP 79* | 92.80 | 16 | 5/1 | 7/3 | 4.1 | 8.2 | .62 | .16 | NI | JH4 |
| 13 | VH4 | DP 65 (42) | 100 | 0 | 0/0 | 0/0 | .0 | .0 | 1,000 | 1,000 | DN4 | JH6 |
| 14 | VH4 | DP 79* | 93.20 | 15 | 5/0 | 5/5 | 3.9 | 7.7 | .180 | .082 | NP | JH4 |
| Case . | Sequence . | Germline VH Gene (reference) . | % Identity . | N . | Obs R/S . | Exp R CDR . | Exp R FR . | p CDR . | p FR . | Germline DH Gene . | Germline JH Gene . | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CDR . | FR . | |||||||||||
| 1 | VH4 | DP 79* | 97.70 | 5 | 2/0 | 1/2 | 1.3 | 2.6 | .273 | .134 | Dxp′1 | JH4 |
| 2 | VH4 | DP 71 (42) | 93.10 | 15 | 0/2 | 3/10 | 3.6 | 7.9 | .018 | .007 | D1 | JH4 |
| 3 | VH1 | DP 25 (42) | 96.40 | 8 | 4/0 | 3/1 | 1.9 | 4.4 | .075 | .075 | Dxp′1 | JH6 |
| 4 | VH3 | DP 77* | 97.80 | 6 | 1/2 | 2/1 | 2.7 | 1.2 | .401 | .401 | DN1 | JH5 |
| 5 | VH4 | DP 66 (42) | 93.20 | 9 | 0/3 | 4/2 | 2.1 | 5.2 | .073 | .234 | Dxp 4 | JH6 |
| 6 | VH4 | DP 65 (42) | 92.70 | 19 | 2/2 | 8/7 | 4.9 | 9.3 | .100 | .154 | Dxp 1/D21/Dxp 4 | JH6 |
| 7 | VH4 | DP 63 (42) | 97.30 | 6 | 2/0 | 2/2 | 1.5 | 3.2 | .299 | .203 | NI | JH6 |
| 8 | VH1 | DP 10 (42) | 96.50 | 8 | 1/2 | 1/4 | 1.9 | 4.4 | .276 | .276 | D21-9/D21-7 | JH6 |
| 9 | VH3 | V4-34 (43) | 96.76 | 7 | 4/0 | 1/2 | 1.8 | 3.6 | .060 | .047 | NI | JH4 |
| 10 | VH4 | DP 49 (44) | 96.80 | 7 | 2/1 | 3/1 | 1.7 | 3.8 | .310 | .240 | NI | JH4 |
| 11 | VH3 | COS 16* | 92.44 | 17 | 9/0 | 5/3 | 3.9 | 9.3 | .006 | .031 | NI | JH4 |
| 12 | VH4 | DP 79* | 92.80 | 16 | 5/1 | 7/3 | 4.1 | 8.2 | .62 | .16 | NI | JH4 |
| 13 | VH4 | DP 65 (42) | 100 | 0 | 0/0 | 0/0 | .0 | .0 | 1,000 | 1,000 | DN4 | JH6 |
| 14 | VH4 | DP 79* | 93.20 | 15 | 5/0 | 5/5 | 3.9 | 7.7 | .180 | .082 | NP | JH4 |
GenBank accession numbers of the sequences, respectively: U86364,U86367, U86370, U86371, U86363, U86366, U86369, U86372, AF004938,AF004937, AF004935, AF004940, AF004936, AF004939.
Abbreviations: VH gene, IgH variable gene; DHgene, IgH diversity gene; JH gene, IgH junction gene; N, total number of mutations observed; R, replacement mutations; S, silent mutations; CDR, complementarity determining region; FR, framework region; p CDR, probability that excess or scarcity of the R mutations in the VH gene CDRs resulted from chance only; p FR, probability that excess or scarcity of the R mutations in the VH gene FRs resulted from chance only; NI, no gene identified with certainty; NP, no gene present.
These germline sequences have not been published but are included in the V BASE sequence directory; all other abbreviations refer to the codes of the previously published germline genes.
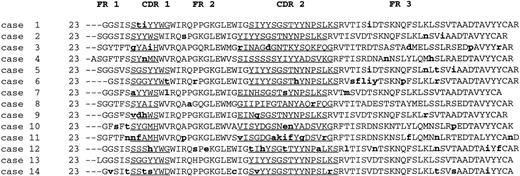
Deduced protein sequences of the rearranged Vh genes of the cases of marginal zone lymphomas. Lowercase, replacement mutations with regard to the germline sequences. FR, framework; CDR, complementarity determining region. CDR regions are underlined.
Deduced protein sequences of the rearranged Vh genes of the cases of marginal zone lymphomas. Lowercase, replacement mutations with regard to the germline sequences. FR, framework; CDR, complementarity determining region. CDR regions are underlined.
Mutation analysis.
The mutation analysis data are summarized in Table 2. In all but one case, the sequences of the rearranged IgH genes contained point mutations with respect to the closest germline sequences. These mutations are most likely due to somatic mutations and are not introduced by the Taq polymerase, as direct sequencing of the PCR products was performed. As such, any Taq polymerase-introduced errors are masked. It cannot be excluded that some of the so-called mutations may actually represent germline polymorphisms. However, these are likely few because most of the human Vhgermline genes have been identified.19
Thirteen cases of marginal zone lymphoma showed point mutations in their rearranged IgH genes. Analysis demonstrated statistically significant evidence for positive antigen selection in case 11 only, originating in the orbit. In that case, more replacement mutations than expected were observed in the CDR regions, as compared with the FR regions. Statistically significant evidence for negative antigen selective pressure was seen in two cases, cases 2 and 9, a marginal zone lymphoma of the spleen and stomach, respectively. In these cases, fewer replacement mutations than expected were observed in the FR regions, indicating antigen selective pressure to maintain the germline configuration. In the other 10 cases with somatic mutations, no statistically significant evidence for antigen selection was observed. The Vh gene of case 13, localized in the skin, was in germline configuration.
DISCUSSION
Our study shows that marginal zone cell lymphomas predominantly rearrange the Vh4 gene family and, to a lesser extent, the Vh3 and Vh1 gene families, in contrast to peripheral blood B cells. A biased Vh gene family usage with respect to the peripheral blood cell repertoire has previously been observed in defined non-Hodgkin's lymphoma subtypes.20-24 In some studies, including some on the MALT lymphomas of the gut and salivary gland, an overrepresentation of only a few of the Vh genes within these families accounts for this bias. These overrepresented Vh genes frequently seem to be involved in auto-antibody production (eg, agglutinins, rheumatoid factors, and anti-DNA antibodies).20,22,23,25 This finding suggests that these B-cell non-Hodgkin's lymphomas may arise from autoreactive B cells. This hypothesis cannot be tested by the analysis of our cases of MALT lymphoma because the number of cases localized to specific sites is too small. However, the hypothesis does not seem valid, at least for the marginal zone cell lymphomas of the spleen and lymph node in our study, because no restricted use of any particular Vhgene was noted. Alternatively, the bias with respect to the usage of Vh genes belonging to certain Vh gene families in marginal zone lymphoma may be explained by the preferential use of certain Vh families by subsets of B cells out of which the lymphoma arises. Indeed, certain compartments of rodent B cells show a bias of the Vh gene family usage, irrespective of selection by antigen.26 Further analysis of Vh gene usage in normal marginal zone B-cell subsets is needed to test this hypothesis.
All cases of splenic marginal zone lymphoma in our study showed somatic mutations in their rearranged Vh genes. One of the cases showed statistically significant evidence of antigen selective pressure against replacement mutations in the rearranged Vh gene to maintain the germline configuration. The presence of somatic mutations in the rearranged Vh genes with evidence of antigen selection has also been reported in splenic lymphoma with villous lymphocytes (SLVL).27 However, the rearranged Vh genes of the cases of SLVL reported showed evidence of positive antigen selection and were present in most cases, in contrast with the findings in our cases of splenic marginal zone lymphoma. SLVL is a B-cell lymphoma that usually presents with splenomegaly.28 The morphology of the leukemic cells, the immunophenotype, and cytogenetics are well characterized, but the relationship of SLVL to the marginal zone cell lymphomas of the spleen is still debated.3,8,27-30 SLVL has been argued to represent the leukemic counterpart of marginal zone cell lymphoma.29 30 Although the number of cases studied is small, the data with respect to the pattern of somatic mutations in the rearranged Vh genes indicate that marginal zone cell lymphoma and SLVL might arise from different subsets of B cells within the spleen, that is, predominantly early and late memory cells, respectively.
Recently, a Vh gene mutation analysis of 5 cases of marginal zone cell lymphomas of the monocytoid B-cell type was performed by Küppers et al.31 Four of their cases showed somatic mutations in the Vh genes with characteristics of positive antigen selection. These findings contrast with the absence of evidence for antigen selection in our cases of monocytoid B-cell lymphoma or marginal zone lymphoma of the lymph node. It is difficult to compare their findings with ours, however, because the primary localization of their lymphoma cases was not reported. At least one of their cases of monocytoid B-cell lymphoma did apparently not localize to the lymph node, but to the stomach.
In our series, two MALT lymphomas that localized to the stomach and to the orbit showed evidence of negative or positive antigen-driven selection, respectively, whereas three MALT lymphoma cases showed somatic mutations in the Vh genes but no evidence of antigen selection. The rearranged Vh gene of the sixth MALT lymphoma case, presenting in the skin, did not contain any somatic mutation. Our findings are similar to the heterogeneous data previously reported for the MALT lymphomas.22-25 The four cases of low-grade MALT lymphomas studied by Qin et al22 and two of a total of six MALT lymphomas reported in two studies conducted by Du et al23,24 showed a VH gene mutation pattern indicative of positive antigen selection. In a recent analysis of five MALT lymphoma cases of the salivary gland, Bahler et al25found somatic mutations in the rearranged Vhgenes, but no statistically significant evidence of antigen selection could be documented.
The occurrence of somatic mutations, in the absence of apparent antigen selection, as observed in most of the marginal zone lymphomas studied in this report, might indicate that an early memory cell of the TD immune reaction (ie, a cell that has not undergone multiple rounds of antigen selection in the germinal center) is the cell of origin of these lymphomas.32 Interestingly, it was recently shown that the normal human marginal zone harbors such cells with a low level of somatic mutations, which are presumed to be early memory B cells.13 It has been postulated that these memory cells are similar to a recently identified peripheral blood IgM-expressing B-cell population that displays a similar pattern of somatic mutations in its rearranged VH genes.33 Alternatively, these cells, with a low level of somatic mutations, might be memory cells involved in the TI immune reaction. However, there is no compelling evidence that the hypermutation mechanism in humans is activated in TI immune reactions, which do not involve the germinal center.34,35 This is in contrast with the findings inXenopus and sheep, where somatic mutations may occur outside the germinal center. In these species, these somatic mutations contribute to the diversification of the antibody repertoire.36 37
At least a subset of the marginal zone lymphomas likely arises from late memory cells showing affinity maturation. Such cells are indeed present in the marginal zone of the spleen and Peyer's patch.13 14 Whether such cells are also present in the marginal zones of the acquired mucosal lymphoid tissues in other organs has not been studied.
One patient with a MALT lymphoma that had originated in the skin showed no mutations in the rearranged Vh gene. These data are similar to those obtained in mantle cell lymphoma and chronic lymphocytic leukemia and suggest that the cell of origin of this case of MALT lymphoma is a naive pregerminal center B cell.38,39 Interestingly, the lymphoma cells of this MALT lymphoma case expressed IgM and strongly IgD, in keeping with such a hypothesis. Naive pregerminal center B cells are predominantly present in the splenic marginal zone of young persons.40 Their presence in the adult marginal zone or in tissues other than the spleen has not been documented.
Whether antigenic stimulation plays a role in the lymphomagenesis and cell growth of marginal zone cell lymphomas is unclear. There is good evidence that this is the case for at least a subset of the MALT lymphomas of the gut, where chronic Helicobacter pyloriinfection may be involved.41 42 However, the absence of statistically significant evidence of positive or negative antigen selection in many of our cases might indicate that antigen does not play a major role in lymphomagenesis and tumor growth in those cases. The use of different Vh genes, such as seen within our series of lymph node-based or spleen-based marginal zone cell lymphomas, at least indicates that no common antigen appears to be involved.
In conclusion, the rearranged Vh genes of the marginal zone cell lymphomas belong primarily to the Vh4, Vh3, and Vh1 families. Somatic mutations occurred in the Vh genes of 13 cases, whereas these were absent in one case. Evidence for antigen-driven selection was observed in only three cases. These data indicate that marginal zone cell lymphomas may originate from distinct subsets of marginal zone B cells, that is, virgin B cells and early as well as late memory B cells.
ACKNOWLEDGMENT
We thank S. Taelemans for excellent technical assistance.
Supported by Nationaal Fonds voor Wetenschappelijk Onderzoek (NFWO) Grant No. G-0311-97.
Address reprint requests to J. Delabie, MD, Department of Pathology II, University Hospitals of Leuven, Minderbroedersstraat 12, B-3000 Leuven, Belgium.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal