Abstract
Diaspirin cross-linked hemoglobin (DCLHb) is an intramolecularly cross-linked hemoglobin-based oxygen carrier being developed as a therapy for acute blood loss. We report here the absence of immunogenicity of DCLHb in patients enrolled in phase II and III clinical trials of DCLHb. Two very sensitive immunoassays, an enzyme-linked immunosorbent assay (ELISA) and a Western blot assay, were developed and validated for this assessment. The DCLHb-antibodies used in these assays were raised in monkeys, had similar affinities for DCLHb and native human hemoglobin (SFHb), and showed cross-reactivity for subunits of DCLHb and SFHb on the Western blot, suggesting that these antibodies were elicited as a xenogenic response to the protein. In the ELISA, the optical density of a patient sample exposed to DCLHb-coated wells was compared with that of the patient sample exposed to carbonate buffer-coated wells; an optical density ratio of 1.4 was established for discriminating between a positive (reactive) or negative DCLHb antibody response. To date, all of the more than 300 patient specimens (preinfusion and postinfusion) from clinical trials have exhibited a ratio of less than 1.4, confirming the lack of preexisting antibodies to DCLHb and clearly showing the absence of DCLHb antibodies after exposure to this new biologic entity. There has been no requirement for use of the confirmatory Western blot assay. Taken together, the results from this study indicate DCLHb is not immunogenic in humans at doses evaluated clinically.
THE SEARCH FOR A temporary red blood cell replacement has been pursued for decades.1,2 Historically, this search has focused on the development of fluids that could be used in place of blood, primarily to reduce concerns about its availability and safety.2 3 However, in recent years, the objectives of this search have changed, and today, the goal is the development of a therapy that will restore both oxygen delivery and perfusion after either global or focal oxygen deficit. This more comprehensive objective has the potential to encompass clinical applications that range from the more traditional uses of blood for resuscitation after acute, severe hemorrhage, in which blood transfusion is the current standard of care, to future applications as a treatment for the ischemia associated with myocardial infarction or stroke, in which blood is not indicated.
Hemoglobin, the iron-containing protein that transports oxygen from the lungs to the tissues, was a natural candidate for use as a red blood cell substitute. In the red blood cell, hemoglobin reversibly binds and releases oxygen via a conformational change from a high-affinity to low-affinity state that is facilitated by the polyanionic effector, 2,3-diphosphoglycerate. However, purified acellular hemoglobin, also known as stroma-free hemoglobin (SFHb), lacks this capability in the absence of an effector. In addition, SFHb dissociates into αβ-dimers that are filtered in the glomerulus of the kidney; high concentrations of dimers overwhelm the filtration capacity of this organ and are toxic. The combination of nephrotoxicity and high oxygen-binding affinity renders SFHb not clinically useful.4 5
The shortcomings of SFHb may be corrected by chemical modification of hemoglobin. For example, covalent cross-linking of purified human hemoglobin by the cross-linking agent, bis(3,5-dibromosalicyl) fumarate (DBBF), in the presence of the polyanion tripolyphosphate has been shown to yield an intramolecularly cross-linked hemoglobin called diaspirin cross-linked hemoglobin (DCLHb).6,7 DCLHb has an oxygen-binding capability comparable to hemoglobin in fresh, whole blood. In addition to its therapeutically useful oxygen-carrying properties, DCLHb functions as an active oncotic and pharmacologic agent. Preclinical and clinical studies indicate that DCLHb is capable of restoring blood pressure, tissue oxygenation, and circulation after acute hypotension after insults such as hypovolemic shock.8Moreover, preclinical studies suggest that DCLHb may be useful in restoring and maintaining perfusion of key organs after myocardial infarction, stroke, or septicemia.8 9
Proteins administered parenterally to achieve therapeutic benefits may concomitantly initiate immune responses.10 As a general rule, the potential for immunogenicity is increased when the secondary or tertiary structure of the modified protein or the charge on the surface of the protein differs from the corresponding properties of the endogenous entity. Native hemoglobin is generally viewed as a nonantigenic protein,11 but, because DCLHb is a chemically modified hemoglobin, a novel epitope(s) may have been introduced that potentially can be immunogenic, either as a direct result of the chemical modification or due to indirect modification of the protein. The generation of an antibody response would cause more rapid clearance of the product, reducing its effectiveness, and may also lead to hypersensitivity reactions, thereby affecting the outcome of clinical studies.
The immunogenicity of DCLHb was first evaluated as a part of the preclinical safety assessment of DCLHb. In one preclinical safety study, a 500 mg/kg dose of DCLHb was infused into five rhesus monkeys at monthly intervals for 5 months.12 No immediate or delayed reactions to the infusions were observed. All serum samples were negative for anti-DCLHb IgG and IgM. Skin testing with two concentrations of DCLHb was also negative. Thus, repeated infusions of DCLHb at this dose did not cause immediate, antibody-mediated, or delayed cellular immune reactions in these primates.
One of the challenges in testing for the presence of DCLHb antibodies is the development and validation of sensitive immunoassays that discriminate between reactive and nonreactive samples. In the present study, we describe the development of such immunoassays, together with the characterization of DCLHb-antibodies raised in monkeys. In addition, we have summarized evaluations of the immunogenicity of DCLHb using these immunoassays, which were completed as a part of more comprehensive patient monitoring in phase II and III clinical trials of DCLHb.
MATERIALS AND METHODS
Materials.
DCLHb 10% and electrolyte injection (lot no. 94D01AD11) and SFHb were manufactured by Baxter Healthcare Corp (Deerfield, IL). Biotinylated molecular weight standards, enhanced chemiluminescence (ECL) Western blotting detection reagents, and Hyperfilm-ECL were obtained from Amersham Inc (Arlington Heights, IL). Phosphate-buffered saline (PBS), Tris-buffered saline (TBS), goat antihuman IgG conjugated with horseradish peroxidase (IgG-HRP), ImmunoPure (G) IgG Purification Kit, Emphaze Biosupport medium, Gentle Binding Buffer, p-nitrophenyl phosphate, 5× diethanolamine solution, and Blotto (5% wt/vol) were obtained from Pierce, Inc (Rockford, IL). Goat antihuman IgG-conjugated alkaline phosphatase was obtained from Accurate Chemicals (Westbury, NY). Precast 18% Tris Glycine gels; precut nitrocellulose membranes; Tris-Glycine sodium dodecyl sulfate (SDS) sample, transfer, and running buffers; and Multimark multicolored standards were obtained from Novex (San Diego, CA). Avidin-HRP and Tween 20 were obtained from Bio-Rad (Hercules, CA). Purified monkey IgG was purchased from Sigma (St. Louis, MO). DCLHb antibodies were raised in rhesus monkeys, as reported previously.12 These antisera were used as a positive control for DCLHb antibodies. Pooled normal human serum (NHS) obtained from healthy donors (n=10) served as a negative control for DCLHb antibodies.
Subjects.
The potential for a human immune response to DCLHb was evaluated using 353 sera samples from both DCLHb-treated and control patients (obtained 3 to 8 weeks postinfusion) and 72 preinfusion samples obtained from subjects in phase II and III clinical studies of DCLHb. These studies included both single-dose intravenous infusions of up to 750 mL (75 g) of DCLHb over 24 hours and repeat dose intravenous infusions of a total of as much as 1,000 mL (100 g) of DCLHb over 72 hours (12 doses in total, delivered at 6-hour intervals).
IgG purification.
IgG from monkey sera was purified using the ImmunoPure (G) IgG Purification Kit. The purity (>99%) of this IgG was confirmed by SDS-polyacrylamide gel electrophoresis (SDS-PAGE) performed under reducing and nonreducing conditions. The IgG concentration was determined by UV spectroscopy, using an extinction coefficient of 1.35 (A280 for 1 mg/mL) for IgG molecules.13
Radiolabeling.
The purified IgG from DCLHb-immunized monkey serum and the control monkey IgG were labeled with 125I using the Iodobeads method (Pierce Inc). The control IgG was also labeled to determine the extent of nonspecific binding to the DCLHb affinity column. The specific activity of the labeled IgG from DCLHb antisera and labeled IgG from control monkey sera were 3.1 and 3.3 μCi/μg, respectively.
DCLHb-liganded affinity column preparation.
A DCLHb-liganded affinity resin (DCLHb-affinity resin) was prepared by incubating (overnight at 2°C to 8°C) 1 g of Emphaze Biosupport medium with 1.2 mL of 10 g/dL DCLHb in 0.8 mol/L sodium citrate/0.1 mol/L sodium bicarbonate solution, pH 8.6 (at 25°C). After overnight incubation, the resin was pelleted by centrifugation, and unreacted sites on the Emphaze were quenched with 3 mol/L ethanolamine, pH 9.0. The affinity resin was isolated by filtration and washed with 10 mmol/L PBS and then 1.0 mol/L NaCl. Affinity columns were prepared by mixing 0.5 g of the DCLHb affinity resin with 5 mL of Gentle Binding Buffer. This slurry was added to a 5-mL column (supplied with the Emphaze kit) and equilibrated with 5 mL of Gentle Binding Buffer.
Active DCLHb antibody concentration.
Estep et al12 have reported raising antibodies against DCLHb in rhesus monkeys. However, attempts to affinity purify this antibody in its active form were not successful. Therefore, the active anti-DCLHb antibody concentration in immunized monkey sera was determined using an adsorption technique wherein approximately 1,000,000 CPM of labeled 125I-IgG from antisera or control monkey 125I-IgG was applied to DCLHb-affinity columns, which were prepared in triplicate. Each column was eluted successively with 5 mL of Gentle Binding Buffer and 6 mL of 1.0 mol/L NaCl. Fraction (1.0 mL) collection was initiated immediately and also followed all wash steps. The radioactivity in each fraction and in the affinity resin was counted using a gamma counter. As a result of this treatment, 1.95% of the radioactivity in the labeled IgG from the DCLHb antisera bound to the DCLHb affinity resin. After identical treatment, 0.70% of the radioactivity from the control IgG bound to the resin, corresponding to the nonspecific binding. After correction for this nonspecific binding, the percentage of active anti-DCLHb antibody was used to calculate the DCLHb-specific antibody concentration in the IgG fraction and in the antisera (74.0 μg/mL).
ELISA.
Estep et al12 have reported the development of a solid-phase ELISA to detect DCLHb-specific antibodies. Although this assay was able to detect DCLHb antibodies, improvements in the assay were necessary to decrease the nonspecific binding, to increase the sensitivity, and to facilitate the validation of the ELISA for the analysis of patient samples from clinical studies. Experimental conditions were optimized with respect to the selection of antigen-coating buffer, blocking buffer, serum diluent, substrate diluent, incubation time for the substrate, and substrate quenching solutions. (See below for details.) As a result of these changes, the nonspecific binding of serum proteins to the antigen decreased by more than twofold. Moreover, the sensitivity for detecting DCLHb antibodies increased by more than 10-fold (data not shown).
All incubations were performed at room temperature, except when noted. All wash steps were performed with PBS-Tween, a 0.05% vol/vol solution of polyoxyethylene sorbitan monolaurate (Tween 20) in PBS. Carbonate buffer, pH 9.6, was used to prepare 1 μg/mL stock solutions of DCLHb. For testing, 100 μL of carbonate buffer (negative control) and each antigen solution were placed in separate wells of 96-well, flat-bottomed microtiter plates. After overnight incubation at 4°C, the ELISA plates were washed and then blocked with 150 μL Blotto for 2 hours at 4°C. Each patient serum sample (diluted 1:100) and control was diluted in 33% Blotto in TBS. After washing of the plates, 100 μL of a sample or control solution was added; all determinations were performed in triplicate. The plates were then incubated for 1 hour. The wells were washed, 100 μL of alkaline phosphatase-labeled antihuman IgG (diluted 1:10,000) was added to each well, and the plates were incubated for 30 minutes. The plates were washed again, 100 μL of p-nitrophenyl phosphate was added to each well, and the plates were incubated for 45 minutes. After 45 minutes, the reaction was quenched with 50 μL of 2 N NaOH, and the optical density of each well was read at 405 nm using a Dynatech plate reader.
ELISA validation.
To monitor a large number of patients for an antibody response to DCLHb and to provide quantitative results, the ELISA was validated. In this validation, a cutoff value was defined for discriminating between a positive and a negative antibody response. The validation study design incorporated both a determination of the sensitivity of the ELISA and a determination of the precision; the latter considered variability due to analysis (n = 3), days (n = 5), and ELISA plates (n = 3). The sensitivity of the assay was defined as the lowest detectable optical density reading that was higher than the optical density reading of a normal population before exposure to DCLHb. To identify this value, serial dilutions from 1:25 to 1:12,800 of the positive control (DCLHb antisera) and the negative control (pooled NHS) were assayed. The optical density measurements were normalized as a ratio of the geometric mean of the value obtained for the positive control relative to that of the negative control (pooled NHS) and subjected to statistical analysis.
Western blot.
The Western blot assay comprised the following steps. DCLHb was separated by SDS-PAGE (18% gel) and was then electrophoretically transferred to a nitrocellulose membrane. The remaining binding sites on the membrane were blocked with Blotto in PBS overnight at 4°C. The membrane was then washed with 50% Blotto in PBS with 0.1% Tween. The membrane was cut into strips exposed to positive control (DCLHb antisera), negative control (NHS), and patient sera specimens. After washing of the membrane strips, the antigen-antibody binding on the membrane was visualized by incubation of the sample strips to IgG-HRP (diluted 1:5,000). This antibody reacts with monkey IgG. The HRP was detected with ECL, using short exposure to blue-light sensitive autoradiography film (Hyperfilm-ECL) to detect the light emitted.
Kinetics.
All kinetic studies were performed using the IAsys resonant mirror biosensor technique (Affinity Sensors, Cambridge, UK) described in detail. 14,15 The IAsys was connected to a circulating waterbath set at 25°C. All samples and buffers were allowed to equilibrate to 25°C before use. All samples were in PBS- Tween, and the reaction volume was 200 μL. For kinetic analysis, the resonant angle was sampled every 0.2 seconds. Data were collected using the IAsys software and analyzed with FASTfit software (Affinity Sensors).
The IAsys uses a cuvette system in which individual cuvettes are placed into and removed from the sensing chamber. Each cuvette incorporates the resonant mirror device, the sensing surface (in these experiments, a carboxymethylated dextran hydrogel), and a reaction chamber with a working volume of 50 to 200 μL. Each cuvette also contains a propeller that efficiently stirred the contents of the reaction chamber. (In all experiments described here, the stirring rate was set at 4,125 rpm.) The temperature in the sensing chamber was maintained at that of the circulating waterbath. Samples were added directly to the cuvette using a pipette and evacuated by means of a tube attached to a peristaltic pump.
DCLHb was coupled to the biosensor surface via the ε-amino groups of lysine residues on the protein using the following procedure. The cuvette was equilibrated with 200 μL of PBS-Tween for 5 to 10 minutes. The surface was then activated by adding 200 μL of both 0.2 mol/L 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDC) and 0.05 mol/L N-hydroxysuccinimide and equilibrating the resulting solution for 8 minutes. The cuvette was washed with PBS-Tween, and 200 μL of 50 μg/mL DCLHb in 10 mmol/L sodium acetate buffer (pH 6.0) was added. This pH was chosen from preliminary experiments as being optimal for maximizing the electrostatic interactions of DCLHb with the hydrogel. After 15 minutes of reaction, the cuvette was washed, 200 μL of 1 mol/L ethanolamine, pH 8.5, was added, and the reaction was continued for 2 minutes to block activated carboxyl groups that had not reacted with DCLHb. SFHb was coupled to surface in the same manner except that the concentration was 5 mg/mL SFHb.
After coupling of protein to the surface, the cuvette was equilibrated with 180 μL of PBS-Tween for 5 to 10 minutes, and then 20 μL of IgG preparation was added. IgG association was monitored for 5 minutes using the IAsys biosensor. The cuvette was washed three times with PBS-Tween (200 μL), and the IgG dissociation was monitored for 5 minutes. The cuvette was regenerated by equilibrating with 200 μL of Gentle Elution Buffer for 2 minutes.
RESULTS
DCLHb antibody characterization.
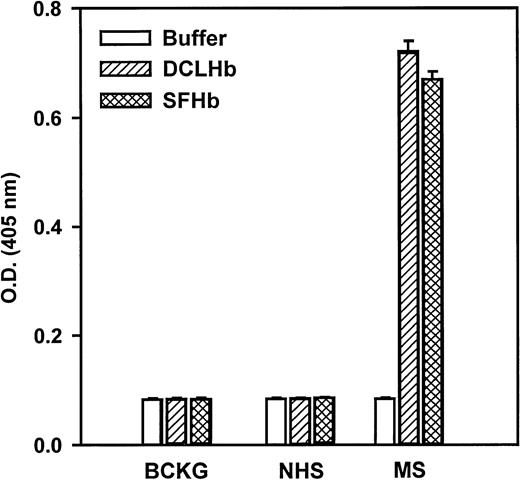
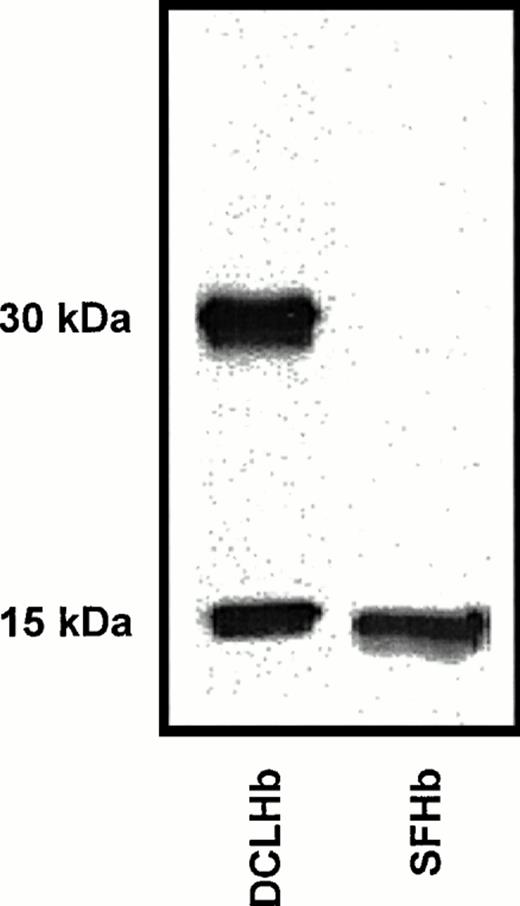
The interactions of DCLHb antibodies (raised in rhesus monkeys) with DCLHb and SFHb were investigated using ELISA, Western blot, and biomolecular interaction analyses. The DCLHb-specific antibodies recognized both DCLHb and SFHb in the ELISA (Fig 1) and Western blot (Fig 2). Western blot results indicated that DCLHb-specific antibodies recognized epitopes on both the αα–cross-linked and β-subunits of DCLHb. This Western blot pattern was consistent with the characteristic pattern for DCLHb on SDS-PAGE, in which bands at approximately 31 kD (αα–cross-linked subunit) and 15 kD (β-monomer) were observed. Note that the antibodies cross-reacted to SFHb but that only a single band was observed at the approximately 15-kD marker. This result also was expected, because both the α- and β-subunits of SFHb have similar molecular weights (∼15 kD).
Specificity of DCLHb antibodies in the ELISA. The concentrations of DCLHb and SFHb were 10 μg/mL. Monkey serum (MS) and NHS were diluted 1:100.
Specificity of DCLHb antibodies in the ELISA. The concentrations of DCLHb and SFHb were 10 μg/mL. Monkey serum (MS) and NHS were diluted 1:100.
Cross-reactivity of DCLHb antibodies to SFHb and DCLHb as assessed by Western blot. The concentrations of DCLHb and SFHb were 1 μg/mL. Monkey serum was diluted 1:100.
Cross-reactivity of DCLHb antibodies to SFHb and DCLHb as assessed by Western blot. The concentrations of DCLHb and SFHb were 1 μg/mL. Monkey serum was diluted 1:100.
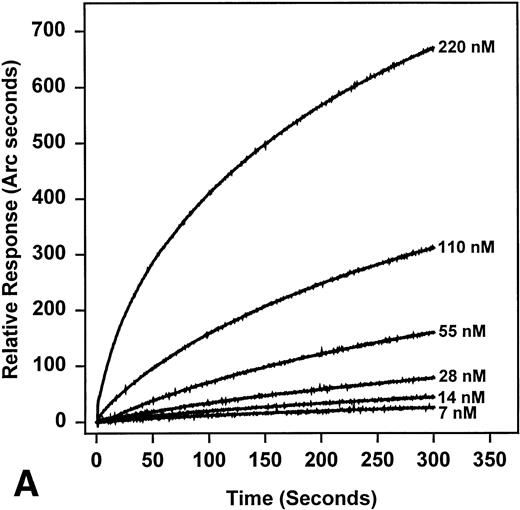
Association rates were determined using pseudo first order conditions by addition of antibody at different concentrations. Typical profiles for the binding of anti-DCLHb antibodies to amine coupled DCLHb are shown in Fig 3A. All of these curves fitted to the following equation for monophasic interactions (for its derivation, see George et al16):
Concentration dependence of the association of antibodies to DCLHb (A) and plot of kobsversus DCLHb concentration (B).
Concentration dependence of the association of antibodies to DCLHb (A) and plot of kobsversus DCLHb concentration (B).
where Rt is the response at time t,kobs is the observed rate constant for the binding, and E is the extent of the reaction (or R at t = ∞).
It should be noted that this approach is designed to determine the kinetics of monoclonal interactions. However, in cases in which a good fit of the data is obtained, it is reasonable to assume that the experimental results represent an average affinity, even with polyclonal antibodies.
Figure 3B shows that kobs has a linear dependence on antibody concentration, a criterion allowing for the determination of the association rate constant (ka) from this plot using equation 2:
In theory, the intercept obtained from this equation equals the dissociation rate constant (kd); however, this value typically incorporates large errors. Therefore,kd was measured directly, and this value was fitted to the equation below.
Average ka and kd values of 2.2 ×104 mol/L−1sec−1 and 5.3 × 10−4 sec−1, respectively, were obtained for DCLHb, giving an average kd of 2.4 ×10−8 mol/L. Similar ka(4.7 × 104 mol/L−1sec−1), kd (4.3 × 104 sec−1), and an averageKd (9 × 10−9 mol/L) were observed for SFHb.
It should be noted that these figures represent an average, because the antiserum is polyclonal in nature. However, in this case, the fit to monophasic binding kinetics was good, suggesting that this approach provides a reasonable estimate. This average affinity for the DCLHb antibodies isolated from primate sera suggests that immunoassays developed using these antibodies provide the sensitivity needed for detecting antibodies in patient sera. No binding of control monkey IgG was seen in these experiments (data not shown), and no binding was seen to an irrelevant antigen (saporin)16 immobilized in the place of DCLHb.
Establishment of positive/negative cutoff value for ELISA.
To discriminate between a positive and a negative antibody response, a cutoff value was defined for the DCLHb antibody ELISA. When establishing a cutoff ratio, it was important to minimize both false-positives and false-negatives. Therefore, it was appropriate to consider both the lower tolerance limit for a positive antibody response (using the monkey DCLHb antisera as the positive control) and the upper tolerance limit for a negative antibody response (using NHS as the negative control).
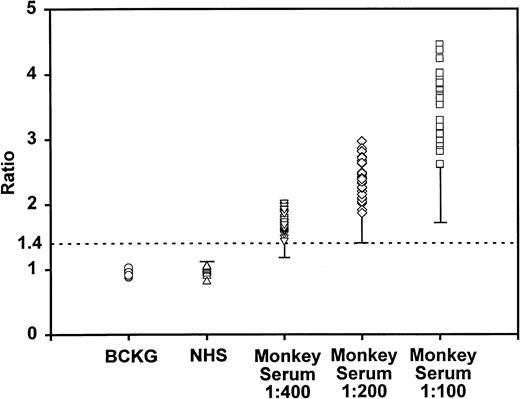
Figure 4 shows the results for the DCLHb antisera at various dilution factors, NHS, and the background expressed as ratios. Several noteworthy inferences may be drawn from an examination of Fig 4. First, it was immediately clear that the ratios of NHS-D (NHS applied to DCLHb-coated wells) to NHS-C (NHS applied to carbonate buffer-coated wells) was similar to the background ratios, suggesting that nonspecific binding of serum Ig proteins to DCLHb did not occur. Second, as expected, higher ratios were observed at each progressively lower dilution factor of the monkey antisera. Third, at a 200-fold dilution of the antisera, a separation between the positive (monkey antisera) and negative antibody response (NHS) was observed. Analysis of these data showed that, at a dilution factor of 200-fold and 400-fold, the average optical density ratio was 2.40 and 1.75, respectively. At these dilutions, the lower tolerance limits for a positive antibody response (99.5% of the population, 90% confidence) were 1.4 and 1.17, respectively.
Statistical evaluation of positive to negative cutoff ratio. The BCKG ratio is the OD ratio of buffer applied to ELISA wells relative to that of NHS (100-fold dilution) applied to carbonate buffer-coated wells. The NHS ratio is the OD ratio of NHS (100-fold dilution) applied to DCLHb-coated wells relative to that of NHS applied to carbonate buffer-coated wells. The monkey serum ratios are the OD ratios of monkey serum (at different dilution factors) applied to DCLHb-coated wells relative to that of NHS applied to carbonate buffer-coated wells. The lower tolerance limit for the positive DCLHb antibody (monkey serum) and upper tolerance for the negative DCLHb antibody responses are shown. The displayed data are the results from all analyses (including those having multiple analysts, assays, plates, etc).
Statistical evaluation of positive to negative cutoff ratio. The BCKG ratio is the OD ratio of buffer applied to ELISA wells relative to that of NHS (100-fold dilution) applied to carbonate buffer-coated wells. The NHS ratio is the OD ratio of NHS (100-fold dilution) applied to DCLHb-coated wells relative to that of NHS applied to carbonate buffer-coated wells. The monkey serum ratios are the OD ratios of monkey serum (at different dilution factors) applied to DCLHb-coated wells relative to that of NHS applied to carbonate buffer-coated wells. The lower tolerance limit for the positive DCLHb antibody (monkey serum) and upper tolerance for the negative DCLHb antibody responses are shown. The displayed data are the results from all analyses (including those having multiple analysts, assays, plates, etc).
An approach analogous to that described above was used to determine the upper limit for the negative antibody response (NHS). However, in this case, a sampling pool of baseline sera samples from 36 patients was deemed sufficient to account for anticipated variability in the patient population. An upper tolerance limit of 1.12 on the negative antibody response was determined using these patient's baseline samples (Fig4).
The combined use of these confidence values and a consideration of the precision of the assay enabled the establishment of a positive to negative cutoff ratio of 1.4 at a 200-fold dilution factor. Under these conditions, the false-negative and false-positive error rates for the ELISA were less than 1 per 10,000 and less than 1 per billion, respectively. Decreasing the dilution factor to 100-fold, the dilution factor at which patient samples are currently tested, decreased the false-negative rate to 53 per billion, whereas maintaining the false-positive error rate at less than 1 per billion.
A standard curve was generated using the active DCLHb antibody concentration determined earlier (74.0 μg/mL). A limit of quantitation of 50 ng/mL of DCLHb antibody at the cutoff value of 1.4 was derived from this curve. Comparable results were obtained with the antisera obtained from a second immunized monkey and, therefore, are not presented.
Western blot.
It is widely recognized that the Western blot assay is useful in elucidating the specificity of antibodies to their corresponding antigens. To provide an additional confirmatory assay in the event that a DCLHb-reactive patient sample was identified, the ECL Western blot shown in Fig 5 was validated. In this assay, a response was considered positive if a band was visually apparent at either the 31-kD or 15-kD molecular weight marker, and its intensity was similar to that observed for the highest diluted standard. If no bands were observed at both molecular weight markers, the response was considered negative. The sensitivity of the assay was found to be similar to that of the ELISA, because bands were visible to a 4,000-fold dilution factor of the monkey antisera (18.5 ng/mL of DCLHb antibodies).
Typical DCLHb antibody Western blot. One microgram of DCLHb was loaded on an SDS-PAGE gel.
Typical DCLHb antibody Western blot. One microgram of DCLHb was loaded on an SDS-PAGE gel.
Clinical evaluation.
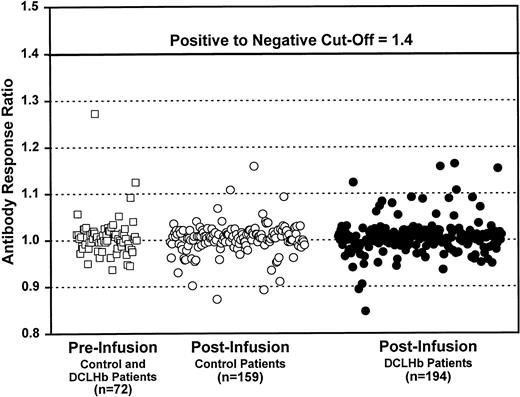
Figure 6 displays the optical density ratios observed from analyses of serum samples from three groups: (1) preinfusion sera samples from subjects receiving DCLHb or the control infusate, (2) postinfusion sera samples from control patients, and (3) postinfusion sera samples from DCLHb patients. ELISA analysis of these samples yielded a combined average optical density ratio of less than 1.4 and average optical density ratios by group of 1.007 ± 0.043, 1.005 ± 0.038, and 1.002 ± 0.032, respectively. These results clearly show that no DCLHb antibodies were detected in any of these patients.
Antibody response in patients exposed to DCLHb or control solution. Antibody response ratio is the OD ratio of patient serum applied to DCLHb-coated wells relative to that of patient serum applied to carbonate buffer-coated wells.
Antibody response in patients exposed to DCLHb or control solution. Antibody response ratio is the OD ratio of patient serum applied to DCLHb-coated wells relative to that of patient serum applied to carbonate buffer-coated wells.
DISCUSSION
This study has shown that no antibodies specific to DCLHb were detected in patient serum samples collected before or after treatment with DCLHb. To our knowledge, this is the first published summary of immunogenicity studies conducted in phase II and III clinical trials of a hemoglobin-based oxygen carrier.
Use of a known titer of a suitable positive control is a prerequisite of any assay to detect or quantify antibodies. However, human hemoglobin A0 is generally viewed as a relatively nonantigenic protein. Moreover, because no patient receiving DCLHb has exhibited a positive immune response to DCLHb, a true positive control for these immunoassays was not available. An assay described by Estep et al12 used antisera raised in rhesus monkeys as the positive control. We also used these antisera as a positive control when testing patient samples.
For routine monitoring of DCLHb antibodies in patients, both primary (ELISA) and confirmatory (Western blot) assays were developed and validated. Many other similar assays that have been described in the literature use a discriminator such as a twofold to threefold ratio above background or 2 to 3 standard deviations above the mean background to differentiate between a positive and a negative.17 This type of analysis usually leads to high errors in the false-positive rates. In contrast, in this study, a cutoff value of 1.4 was based on a statistical evaluation of validation data that incorporated many different factors contributing to the variability in the ELISA. As a consequence, both false-positive and false-negative error rates were very low. Moreover, the ELISA used in this study had a sensitivity sufficient for the quantitation of antibodies to DCLHb at low levels (50 ng/mL).
This ELISA, which detects the clinically relevant antibodies to native (nondenatured) DCLHb, was used in the evaluation of more than 300 patient specimens from clinical trials of DCLHb. These samples included both preinfusion samples from DCLHb-treated and control patients and, more importantly, postinfusion samples from DCLHb-treated patients. All patient sera tested negative for DCLHb-antibodies, confirming the lack of preexisting antibodies to DCLHb and clearly showing the absence of DCLHb antibodies after exposure to this biologic product.
These results are not surprising, because DCLHb is not likely to be immunogenic in humans for several reasons. First, DCLHb is derived from human hemoglobin, and the fumaryl bis(amide) bridge is buried in the central water cavity between the two α subunits of the protein. Structural characterization studies by mass spectrometry18and electronic circular dichroism and fluorescence spectroscopy19 have shown that DCLHb is structurally very similar to native human hemoglobin, with the exception of the internal cross-link; thus, the presence of novel epitopes in DCLHb is not likely. Biomolecular interaction analysis showed that the affinity of DCLHb antibodies for DCLHb was characterized by an average antibody affinity constant in the nanomolar range. A similar affinity constant was observed for SFHb, suggesting that the antibodies raised in rhesus monkeys represented a xenogenic response and not one due to the cross-linker in DCLHb.
In addition, the cross-reactivity of this antibody to SFHb in both the ELISA and the Western blot further supports the conclusion that the specificity of these antibodies was not likely to be directed against the cross-linker or other changes in the structure of molecule caused by this modification. This cross-reactivity of the DCLHb antibodies to SFHb was expected, because the antibodies in the monkey sera were more likely to be polyclonal in nature rather than monoclonal antibodies specific to DCLHb, confirming the polyclonal nature of the DCLHb-specific antibodies.
In a preclinical study using primates, a 500 mg/kg dose of DCLHb was infused at monthly intervals for 5 months; no immediate or delayed reactions to the infusions were observed. In fact, antibody production in these primates was only possible after immunization with adjuvant.12 When these observations are considered together with the pharmacokinetics of DCLHb after acute infusion of DCLHb (a circulating half-life of less than 24 hours), it is reasonable to conclude that DCLHb is not immunogenic in humans.
An earlier in vitro biocompatibility study of DCLHb showed that DCLHb does not activate the complement system and does not induce cytokines.20 These same markers were monitored in the phase I safety study and showed no stimulation of either cascade.21 Taken together, the results from this study and the results reported earlier suggest DCLHb is not immunogenic in humans under conditions in which it would be administered clinically.
Address reprint requests to Mehul J. Patel, PhD, Baxter Healthcare Corp, WG3-2S, 25212 W. State Route 120, Round Lake, IL 60073-9799.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal