Abstract
Differentiation therapy with all-trans retinoic acid (ATRA) has marked a major advance and become the first choice drug in the treatment of acute promyelocytic leukemia (APL). However, patients who relapse from ATRA-induced complete remission (CR) have difficulty in obtaining a second CR with a second course of ATRA therapy alone. We tested the efficacy of a new synthetic retinoid, Am80, in APL that had relapsed from CR induced by ATRA in a prospective multicenter study. Am80 is approximately 10 times more potent than ATRA as an in vitro differentiation inducer, is more stable to light, heat, and oxidation than ATRA, has a low affinity for cellular retinoic acid binding protein, and does not bind to retinoic acid receptor-γ. Patients received Am80, 6 mg/m2, orally alone daily until CR. Of 24 evaluable patients, 14 (58%) achieved CR. The interval from the last ATRA therapy was not different between CR and failure cases. The clinical response was well correlated with the in vitro response to Am80 in patients examined. Adverse events included 1 retinoic acid syndrome, 1 hyperleukocytosis, 9 xerosis, 8 cheilitis, 16 hypertriglyceridemia, and 15 hypercholesterolemia, but generally milder than those of ATRA, which all patients had received previously. Am80 is effective in APL relapsed from ATRA-induced CR and deserves further trials, especially in combination with chemotherapy.
DIFFERENTIATION THERAPY with all-trans retinoic acid (ATRA) has marked a major advance in the treatment of acute promyelocytic leukemia (APL). Several studies have shown that treatment regimens using ATRA for remission induction followed by several cycles of cytotoxic chemotherapy yield a higher remission rate and superior overall survival compared with those produced by chemotherapy alone.1-5 However, the duration of remission induced and maintained by ATRA therapy alone is generally short-lived, and, when relapse occurs, ATRA alone fails to induce a second remission in a majority of patients.6 7
Several mechanisms for this acquired ATRA resistance have been postulated, including accelerated in vivo clearance of ATRA,8 increased levels of cellular retinoic acid binding protein (CRABP),9,10 mutations in retinoic acid receptor-α (RAR-α) gene, and additional genetic abnormalities.6,7 11
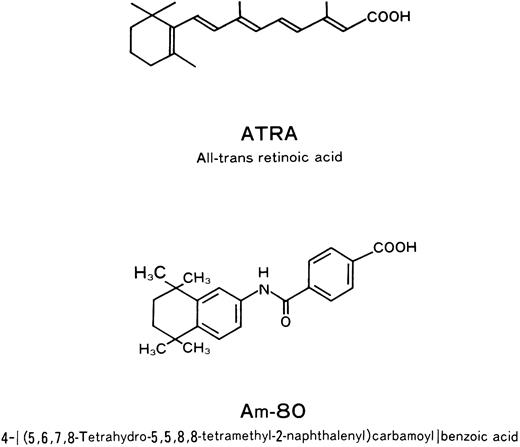
We previously reported that a new synthetic retinoid, Am80 (4 [(5,6,7,8-tetrahydro-5,5,8,8-tetramethyl-2-naphthalenyl) carbamoyl]benzoic acid) (Fig 1),12,13 induced complete remission (CR) in two patients with APL who had relapsed from ATRA-induced CR.14 Am80 is approximately 10 times more potent than ATRA as an in vitro inducer of differentiation in NB-4 and HL-60 cells, is chemically more stable to light, heat, and oxidation than ATRA, has a low affinity for CRABP, and does not bind to RAR-γ.12,13 Therefore, Am80 would be expected to have therapeutic effectiveness in patients with ATRA-resistant APL with increased CRABP, and have less adverse drug reaction related to RAR-γ, which is the major retinoic acid receptor in the dermal epithelium.15
Here we report the result of a multicenter prospective study of Am80 in 25 patients with APL who have relapsed from ATRA-induced CR at the Leukemia Study Group of the Ministry of Health and Welfare.
PATIENTS AND METHODS
From March 1995 to April 1996, 25 patients with APL who had previously obtained CR with daily oral 45 mg/mg2 ATRA therapy alone or in combination with chemotherapy, and subsequently relapsed from the CR during or after the postremission chemotherapy, were prospectively registered from 10 hospitals at the Koseisho Leukemia Study Group. Most patients received a postremission chemotherapy by the AML92 protocol of the Japan Adult Leukemia Study Group.5 Diagnosis of APL was made according to the French-American-British (FAB) classification16,17 and confirmed by the presence of t(15; 17) karyotype and/or PML/RAR-α gene rearrangement. To be eligible, patients should have more than 10% of blasts and promyelocytes in bone marrow (BM), have an Eastern Cooperative Oncology Group (ECOG) performance status 3 or less, have <1 × 109/L blasts and promyelocytes in peripheral blood (PB), lack uncontrollable disseminated intravascular coagulation (DIC), and not be pregnant. After giving written informed consent, patients received a daily oral dose of 6 mg/m2 Am80 alone until CR in two divided doses after meals. The daily dose was permitted to be increased to 9 mg/m2 2 weeks after the start of therapy if there was no satisfactory response, and to be decreased to 3 mg/m2 or discontinued if there appeared serious adverse events. Concomitant use of chemotherapy and/or granulocyte colony-stimulating factor were not allowed. Response was evaluated by standard criteria generally used for chemotherapy.18 CR was defined as less than 5% of blasts and promyelocytes with normal erythropoiesis, thrombopoiesis, and granulopoiesis in the BM, and more than 1.5 × 109/L neutrophils and more than 100 × 109/L platelet in the PB. When patients obtained CR, Am80 was discontinued. Postremission therapy was not specified by the protocol, but allogenic BM transplantation was recommended if HLA-matched donors were available from siblings or unrelated donors. The study was approved by the institutional review board at each hospital.
In some patients, leukemia cells were obtained from BM and cultured with 10−8 mol/L and 10−6 mol/L of Am80 or ATRA for 48 hours, and the in vitro differentiation of leukemia cells was predicted by the restoration of PML and PML-RAR-α subcellular localization from diffuse fine-granular patterns to normal speckled patterns using an immunostaining method reported elsewhere.19,20 In short, purified leukemia cells fixed with periodate-lysine-paraformaldehyde (0.01 mol/L NaIO4 , 0.075 mol/L phosphate buffer, and 2% paraformaldehyde; pH 6.2) were stained with an anti-PML antibody (1:200), which was generated against the N-terminus of PML protein, and fluorescence-labeled goat-anti rabbit IgG (1:100; Kappel, West Chester, PA). The restoration effect was quantified by the method described previously.19 Briefly, we examined 100 cells and determined the percentage of cells with the speckled staining. When an APL cell showed a full restoration to a normal speckled pattern, we counted it as 1. When it showed incomplete speckled staining with fine granules and/or cytoplasmic staining, we counted it as 0.5.
Furthermore, in two healthy volunteers and in several patients, plasma concentration of Am80 was preliminary measured with HPLC-RIA after oral administration of Am80.
RESULTS
One patient died before the delivery of Am80, and thus 24 patients were evaluated. Patient characteristics are summarized in Table 1. Age ranged from 19 to 76 years, with a median of 49 years. There were 13 males and 11 females. Leukocyte counts before the start of therapy ranged from 0.3 to 3.92 × 109/L with a median of 1.3 × 109 /L. Platelet counts ranged form 10 to 153 × 109/L with a median of 71 × 109/L. Blasts plus promyelocytes in the BM ranged from 14% to 96% with a median of 60%. Fibrinogen ranged from 0.68 to 5.7 g/L with a median of 2.23 g/L. The interval from the last day of the prior ATRA therapy to the present Am80 therapy ranged from 3 to 58 months with a median of 22 months. All patients were treated with Am80 as the first treatment after the ATRA-induced CR, except for one patient who had been treated with ATRA for her first relapse 3 months before the Am80 therapy, resulting in no response. Thirteen patients had signs and symptoms of DIC: 2 severe, 5 intermediate, and 6 mild.
Patient Characteristics
| Registered | 25 |
| Not treated | 1 |
| Evaluable | 24 |
| Male/female | 13/11 |
| Age median (range) | 49 yr (19-76) |
| WBC median (range) | 1.3 × 109/L (0.3-3.92) |
| RBC median (range) | 3.59 × 1012/L (2.30-4.46) |
| Platelet median (range) | 71 × 109/L (10-153) |
| Blasts in BM | |
| median (range) | 60% (14-96) |
| Fibrinogen median (range) | 2.23 g/L (0.68-5.37) |
| Interval from the last ATRA | |
| median (range) | 22 mo (3-58) |
| Registered | 25 |
| Not treated | 1 |
| Evaluable | 24 |
| Male/female | 13/11 |
| Age median (range) | 49 yr (19-76) |
| WBC median (range) | 1.3 × 109/L (0.3-3.92) |
| RBC median (range) | 3.59 × 1012/L (2.30-4.46) |
| Platelet median (range) | 71 × 109/L (10-153) |
| Blasts in BM | |
| median (range) | 60% (14-96) |
| Fibrinogen median (range) | 2.23 g/L (0.68-5.37) |
| Interval from the last ATRA | |
| median (range) | 22 mo (3-58) |
Out of 24 evaluable patients, 14 (58%) obtained CR (Table 2). CR was reached between 20 to 58 days after the start of therapy with a median of 41 days. Twelve patients achieved CR with 6 mg/m2 of Am80. One patient received an increased dose of 9 mg/m2 from day 15, and obtained CR on day 28. The other patient showed rapid increase of leukocyte counts from 0.3 × 109/L to 15.3 ×/L, received a reduced dose of 3 mg/m2 from day 7, and obtained CR on day 58. The intervals from the last ATRA therapy were not different between CR and failure cases. The interval ranged from 13 to 45 months with a median of 22 months for 14 CR cases, and from 3 to 58 months with a median of 17 months for 10 failure cases. None of 3 patients who relapsed within 12 months from the last ATRA therapy achieved CR. The ages were not different between two groups, which ranged from 19 to 76 years with a median of 51 years for the CR cases and from 21 to 73 years with a median of 49 years for the failure cases. The initial percentages of blasts plus promyelocytes in the BM were not different between two groups, which ranged from 14% to 94% with a median of 60% for the CR cases, and from 21% to 96% with a median of 58% for the failure cases (Table 2).
Treatment Outcome
| No. of evaluable patients | 24 |
| No. of patients achieving CR | 14 (58%) |
| Day till CR | |
| median | 41 d |
| range | 20-58 d |
| Interval from the last ATRA therapy | |
| In CR patients | |
| median | 22 mo |
| range | 13-45 mo |
| In failure patients | |
| median | 17 mo |
| range | 3-58 mo |
| No. of evaluable patients | 24 |
| No. of patients achieving CR | 14 (58%) |
| Day till CR | |
| median | 41 d |
| range | 20-58 d |
| Interval from the last ATRA therapy | |
| In CR patients | |
| median | 22 mo |
| range | 13-45 mo |
| In failure patients | |
| median | 17 mo |
| range | 3-58 mo |
Although all patients who achieved CR did so without concomitant chemotherapy, two patients who received chemotherapy either before or after Am80 failed to achieve CR. One patient received chemotherapy (40 mg/m2 daunorubicin for 2 days and 200 mg/m2 behenoyl cytarabine for 4 days) starting 6 days before the Am80 therapy to reduce the high peripheral leukemia cell (4.9 × 109L) and to meet the eligibility criteria, but did not achieve CR. Another patient received 140 mg/m2 cytarabine and 10 mg/m2 aclarubicin concomitantly for 7 days from the third week of the Am80 therapy due to the progressive disease, but did not achieve CR. No other patients received chemotherapy before and during the Am80 therapy.
Among 10 failure cases, 3 patients showed progression of the disease and died between 24 and 65 days, and 7 showed either no progression or some improvement but did not fulfill the CR criteria. In 4 failure cases, the dose of Am80 was increased to 9 mg/m2, and later to 12 mg/m2 in 2 patient, but none of them achieved CR. Except for the cases with progressive disease, clinical signs and symptoms of DIC, if present, showed some improvement, even in the failure cases.
In 17 patients, leukemia cells were tested for the in vitro differentiation by Am80 and ATRA before the start of the AM80 therapy (Table 3). The clinical response was fairly well correlated with the in vitro response to 10-8 mol/L Am80. Nine of them achieved CR with the Am80 therapy, and more than 30% of their leukemia cells responded to 10−8 mol/L Am80 and more than 60% to 10−6 mol/L Am80. In 4 of these responders their leukemia cells also responded to 10−8 mol/L ATRA. Patient 10 showed some clinical response for the first 2 weeks, but became nonresponsive afterward.
In Vitro Differentiation of Leukemia Cells From Patients by Am80 and Their Clinical Response to Am80 Therapy
| Patient . | Month . | Blast % . | In Vitro Response (%)3-150 . | |||||
|---|---|---|---|---|---|---|---|---|
| . | From Last . | in . | Am80 . | ATRA . | Clinical . | Day to . | ||
| . | ATRA . | Marrow . | 10−8 mol/L . | 10−6 mol/L . | 10−8 mol/L . | 10−6 mol/L . | Response . | CR . |
| 1 | 30 | 23 | 83 | 92.5 | 77.5 | 94.5 | CR | 20 |
| 2 | 18 | 97 | 70.5 | NT | 74.5 | NT | CR | 46 |
| 3 | 25 | 14 | 72 | 88 | 75.5 | 92.5 | CR | 37 |
| 4 | 22 | 26 | 47.5 | NT | 58 | NT | CR | 41 |
| 5 | 24 | 92 | 75 | 84.5 | 16 | 24.5 | CR | 43 |
| 6 | 18 | 88 | 56.5 | 79.5 | 20.5 | 40.5 | CR | 46 |
| 7 | 22 | 84 | 53.5 | 83 | 20.5 | 39 | CR | 28 |
| 8 | 25 | 14 | 40.5 | 66 | 35 | 60.5 | CR | 40 |
| 9 | 45 | 89 | 34 | 66.5 | 28.5 | 60.5 | CR | 58 |
| 10 | 3 | 67 | 30 | 59.5 | 27.5 | 63 | F | |
| 11 | 14 | 62 | 14 | 63.5 | 15 | 67 | F | |
| 12 | 14 | 96 | 11.5 | 29 | 12 | 32.5 | F | |
| 13 | 20 | 88 | 11 | 30.5 | 8 | 13.5 | F | |
| 14 | 25 | 44 | 9 | 13.5 | 10.5 | 12 | F | |
| 15 | 27 | 82 | 4.5 | 12 | 6.5 | 10.5 | F | |
| 16 | 2 | 25 | 3 | NT | 4.5 | NT | F | |
| 17 | 30 | 96 | 2.5 | 5 | 2 | 2 | F | |
| Patient . | Month . | Blast % . | In Vitro Response (%)3-150 . | |||||
|---|---|---|---|---|---|---|---|---|
| . | From Last . | in . | Am80 . | ATRA . | Clinical . | Day to . | ||
| . | ATRA . | Marrow . | 10−8 mol/L . | 10−6 mol/L . | 10−8 mol/L . | 10−6 mol/L . | Response . | CR . |
| 1 | 30 | 23 | 83 | 92.5 | 77.5 | 94.5 | CR | 20 |
| 2 | 18 | 97 | 70.5 | NT | 74.5 | NT | CR | 46 |
| 3 | 25 | 14 | 72 | 88 | 75.5 | 92.5 | CR | 37 |
| 4 | 22 | 26 | 47.5 | NT | 58 | NT | CR | 41 |
| 5 | 24 | 92 | 75 | 84.5 | 16 | 24.5 | CR | 43 |
| 6 | 18 | 88 | 56.5 | 79.5 | 20.5 | 40.5 | CR | 46 |
| 7 | 22 | 84 | 53.5 | 83 | 20.5 | 39 | CR | 28 |
| 8 | 25 | 14 | 40.5 | 66 | 35 | 60.5 | CR | 40 |
| 9 | 45 | 89 | 34 | 66.5 | 28.5 | 60.5 | CR | 58 |
| 10 | 3 | 67 | 30 | 59.5 | 27.5 | 63 | F | |
| 11 | 14 | 62 | 14 | 63.5 | 15 | 67 | F | |
| 12 | 14 | 96 | 11.5 | 29 | 12 | 32.5 | F | |
| 13 | 20 | 88 | 11 | 30.5 | 8 | 13.5 | F | |
| 14 | 25 | 44 | 9 | 13.5 | 10.5 | 12 | F | |
| 15 | 27 | 82 | 4.5 | 12 | 6.5 | 10.5 | F | |
| 16 | 2 | 25 | 3 | NT | 4.5 | NT | F | |
| 17 | 30 | 96 | 2.5 | 5 | 2 | 2 | F | |
Abbreviations: NT, not tested; F, failure.
The in vitro differentiation of leukemia cells was predicted by the restoration of PML and PML-RAR-α subcellular localization from diffuse fine-granular patterns to normal speckled patterns using an immunostaining method. We examined 100 cells and determined the percentage of cells with the speckled staining. When an APL cell showed a full restoration to a normal speckled pattern, we counted it as 1. When it showed incomplete speckled staining with fine granules and/or cytoplasmic staining, we counted it as 0.5.
In two healthy volunteers, 4 mg per person of Am80 was administered orally, and the plasma concentrations of Am80 were measured up to 24 hours (Table 4). Peak levels of 62 ng/mL (1.6 × 10−7) mol/L and 41 ng/mL (1.2 × 10−7 mol/L) were obtained after 2 to 3 hours of oral administration, and a trace amount was detected at 24 hours in one volunteer. Plasma levels were also preliminarily measured 3 hours after oral administration of Am80 in several patients. After 3 mg/m2 of Am80, 28 and 44 ng/mL of Am80 were observed in 2 patients, respectively; after 4.5 mg/m2, 21 and 71 ng/mL in 2 patients, respectively; after 6 mg/m2, 99 ng/mL in 1 patient. One of them had 44 ng/mL after 3 mg/m2 day 1 and 71 ng/mL after 4.5 mg/m2 on day 24, suggesting that there seemed to be no decrease of the plasma levels of Am80 after continuous oral administration in this patient, who achieved CR on day 28. Approximately 12 hours after 3 mg/m2 administration, namely before the next administration in the following morning, 1.4 to 7 ng/mL of Am80 was detectable in all three patients examined, showing that the plasma clearance of Am80 was rather slow.
Plasma Concentration of Am80 After Single Oral Administration of 4 mg of Am80 per Person in Two Healthy Volunteers
| Age (yr) . | Sex . | Weight (kg) . | Plasma Concentration of Am80 (ng/mL) . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | Before . | 0.5 . | 1 . | 2 . | 3 . | 5 . | 7 . | 24 h . |
| 52 | Male | 65 | <1 | 1.2 | 9.5 | 61.9 | 33.4 | 33.4 | 21.7 | 1.1 |
| 48 | Female | 53 | <1 | 1.6 | 19.0 | 41.3 | 38.0 | 17.3 | 7.8 | <1 |
| Age (yr) . | Sex . | Weight (kg) . | Plasma Concentration of Am80 (ng/mL) . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | Before . | 0.5 . | 1 . | 2 . | 3 . | 5 . | 7 . | 24 h . |
| 52 | Male | 65 | <1 | 1.2 | 9.5 | 61.9 | 33.4 | 33.4 | 21.7 | 1.1 |
| 48 | Female | 53 | <1 | 1.6 | 19.0 | 41.3 | 38.0 | 17.3 | 7.8 | <1 |
Plasma concentration of Am80 was measured with high-performance liquid chromatography.
Adverse effects of Am80 generally were milder compared with those experienced during the previous ATRA therapy. Because all patients had previously received the ATRA therapy, most patients as well as their attending physicians stated that the subjective and objective cutaneous adverse effects were less than those experienced with ATRA. Retinoic acid (RA) syndrome was seen in one patient who presented typical features of this syndrome including fever, dyspnea, low arterial oxygen level, and diffuse opaque pulmonary shadows, but without hyperleukocytosis on day 18. Am80 was discontinued and he was successfully treated with methylprednisolone pulse therapy. He then resumed 3 mg/m2 of Am80 on day 33 and achieved CR on day 46. He did not experience RA syndrome during the previous ATRA therapy. One patients had leukocytosis of 51.2 × 105/L and 3 other patients had moderate leukocytosis between 10 to 16 × 109/L during the Am80 therapy. Higher-than-normal levels of hypertriglyceridemia were seen in 16 patients (>5.0 g/L in 9; maximum, 9.95 g/L), and hypercholesterolemia in 15 (>3.0 g/L in 5; maximum, 11.66 g/L) (Table 5).
Adverse Effects of Am80 Therapy
| . | No. of Cases (%) . | |||
|---|---|---|---|---|
| . | No . | Mild . | Moderate . | Severe . |
| Cheilitis | 16 (67) | 8 (33) | 0 | 0 |
| Xerosis | 15 (63) | 8 (33) | 1 (4) | 0 |
| GI trouble | 22 (92) | 2 (8) | 0 | 0 |
| Bone pain | 19 (79) | 0 | 5 (21) | 0 |
| Headache | 18 (75) | 3 (13) | 3 (13) | 0 |
| Dermatitis | 19 (79) | 0 | 5 (21) | 0 |
| RA syndrome | 23 (96) | 0 | 0 | 1 (4) |
| Liver damage | 21 (88) | 3 (13) | 0 | 0 |
| Hyperleukocytosis | 20 (83) | 3 (13)5-150 | 0 | 1 (4)5-151 |
| Hypercholesterolemia | 9 (37) | 10 (42)5-152 | 4 (17)ρ | 1 (4)5-155 |
| Hypertrigliceridemia | 8 (33) | 2 (8)5-152 | 5 (21)ρ | 9 (38)5-155 |
| . | No. of Cases (%) . | |||
|---|---|---|---|---|
| . | No . | Mild . | Moderate . | Severe . |
| Cheilitis | 16 (67) | 8 (33) | 0 | 0 |
| Xerosis | 15 (63) | 8 (33) | 1 (4) | 0 |
| GI trouble | 22 (92) | 2 (8) | 0 | 0 |
| Bone pain | 19 (79) | 0 | 5 (21) | 0 |
| Headache | 18 (75) | 3 (13) | 3 (13) | 0 |
| Dermatitis | 19 (79) | 0 | 5 (21) | 0 |
| RA syndrome | 23 (96) | 0 | 0 | 1 (4) |
| Liver damage | 21 (88) | 3 (13) | 0 | 0 |
| Hyperleukocytosis | 20 (83) | 3 (13)5-150 | 0 | 1 (4)5-151 |
| Hypercholesterolemia | 9 (37) | 10 (42)5-152 | 4 (17)ρ | 1 (4)5-155 |
| Hypertrigliceridemia | 8 (33) | 2 (8)5-152 | 5 (21)ρ | 9 (38)5-155 |
<20 × 109/L.
≥50 × 109/L.
<3.0 g/L.
ρ 3.0-4.99 g/L.
≥5.0 g/L.
After the achievement of CR, 5 patients received HLA-matched allogeneic BMT (3 from siblings and 2 from unrelated donors) and all remain in CR up to 14 months. One patient was continued on the Am80 therapy and relapsed 2 months later. Another 8 patients received various kinds of chemotherapeutic regimens; 1 relapsed 4 months later and the others remain in CR up to 14 months.
DISCUSSION
Since Chinese investigators first reported more than 90% CR in patients with APL by ATRA therapy, several groups have confirmed the remarkable efficacy of this drug as a differentiation therapy for APL.1-5 Moreover, because ATRA therapy causes less complications than myelosuppressive chemotherapy, the medical costs required during the remission induction therapy are lower in ATRA therapy than in chemotherapy.21,22 Thus, ATRA therapy has become the first choice therapy for APL from both medical and economical points of view.5,23 However, patients who relapse from ATRA-induced CR have difficulty in obtaining a second CR with a second course of ATRA alone.6,7 Patients who relapse while taking ATRA, usually as a maintenance therapy, respond poorly to even a two fold dose escalation of ATRA, and Warrell et al24 reported that none of their 10 patients achieved a second CR by this strategy. Also, even patients who were retreated with ATRA at some point after having ceased ingestion of the drug responded poorly. In our experience, only 3 of 17 patients who relapsed after ATRA-induced CR obtained a second CR by ATRA alone,25,26 and Warrell et al reported that only 3 of 10 such patients obtained a second CR.24 The odds of obtaining a second CR are not related to the time off from prior treatment both in our and their patients. Chinese investigators reported that only 2 of 10 patients who were treated with ATRA alone after ATRA-induced CR survived more than 30 months.27 Therefore, taken together, around 20% of APL patients previously treated with ATRA seem to retain the responsiveness to ATRA alone.
Several mechanisms for acquired resistance to ATRA have been postulated.6 Because continuous oral treatment results in a progressive and sustained decrease in plasma concentrations of ATRA, an insufficient plasma level seems to be one of the mechanisms.8 Proposed explanations for this phenomenon include an increase in cytochrome P450 enzyme activity, which hydroxylates ATRA at the cyclohexenyl ring,28 an increase in other oxidative enzyme activity such as lipid hydroperoxidases,29 and an induction of multidrug-resistance-1 gene to express P-glycoprotein.30 However, because an intermittent schedule of ATRA administration results in repetitive periods of relatively high plasma concentrations of the drug,31 a low plasma level of ATRA alone does not explain all of the acquired resistance, which is generally long-lived.
Another proposed mechanism of the acquired resistance to ATRA is an increased expression of CRABP in ATRA-resistant APL cells.10,32 Overexpression of the CRABP is known to result in accelerated metabolism of retinoic acid, suggesting that the CRABP facilities the delivery of ATRA to the microsomal oxidases that catalyze its degradation.33
Another putative mechanism is the mutation in the RAR-α gene as noted in HL-6034 and NB-4 cells35 as well as the selection of non-APL leukemia clones. However, it seems unlikely that genetic mutations explain all of the mechanisms, because clinical resistance appears almost universally and develops quite rapidly. All patients in the present study had t(15; 17) and/or PML/RAR-α at their relapse.
Am80 was synthesized and kindly provided by Prof K. Shudo (University of Tokyo Faculty of Pharmaceutical Sciences, Tokyo, Japan). The preliminary pharmacokinetic studies were done in rats,14 normal volunteers, and in patients in Prof Shudo's laboratory and, in our laboratory. After oral administration of 3 mg/m2 of Am80, 10−7 mol/L of plasma levels, which are sufficient concentrations for in vitro differentiation of HL-60, NB-4, and APL cells from patients, are easily attained in patients. The levels peaked at 2 to 3 hours, then decreased gradually within the next 4 to 5 hours, and were detectable at 12 hours. More than 99% of Am80 bind to plasma albumin in humans, and are excreted mainly from the bile tract within 48 hours in rats.14 The plasma level of Am80 was proportional to the administered dosage on day 24 in one patient preliminarily tested, indicating that the plasma clearance of this drug may not be accelerated after continuous oral administration.
Several therapeutic strategies intended to overcome resistance to ATRA are currently being studied, but to date this has yielded little success.6,7,11 Miller et al36 recently reported that treatment with 9-cis retinoic acid resulted in only 1 CR among 7 patients with APL who had relapsed from ATRA-induced CR. Because 9-cis retinoic acid does not bind to CRABP,37 their observation implies that the increased CRABP is not the sole cause of ATRA resistance. Concomitant use of ketoconazole or fluconazole, both of which inhibit the oxidative activity of cytochrome P450,38,39 has not been shown to reverse the acquired retinoid resistance. Use of interferon also shows controversial outcomes.40,41 Estey et al42 administered liposome-encapsulated ATRA and found that there were no differences between the area under the curve of ATRA concentration versus time on day 1 and day 15, and even on day 85. Three out of 6 patients, each in the first relapse and at least a year from the last exposure to oral ATRA, achieved CR.42 Thus, if the acquired resistance derives from decreased plasma concentration of ATRA, this liposome-encapsulated ATRA may overcome the resistance. Furthermore, Chinese investigators recently reported that arsenic trioxide was effective in treating APL.43-45 Zhang et al44 reported that the arsenic compound induced CR in 22 of 42 previously treated patients, the majority of whom had relapsed from ATRA-induced CR, and Shen et al45 reported CR in 14 of 15 similar patients.
Treatment with Am80 induced 58% CR in this study in 24 patients with APL who had relapsed from CR that had previously been induced by ATRA and maintained mostly with postremission chemotherapy. There was no correlation between the clinical response and the interval from the last ATRA treatment. It is not clear whether the patients who obtained CR with Am80 did not respond to the second ATRA therapy. In fact, our preliminary in vitro tests showed that APL cells from some of our patients responded to and were differentiated by both 10−8 mol/L ATRA and Am80. However, APL cells from other patients did not respond to 10−8 mol/L ATRA but responded to 10−8 mol/L Am80, and these patients obtained CR with Am80 (Table 3). Therefore, probably about 20% of the relapsed patients from ATRA-induced CR would respond to both Am80 and the second treatment of ATRA alone, and some 30% to 40% of the relapsed patients would respond only to Am80. Because we had no method to examine CRABP in our patients, it is not certain whether Am80 worked on APL with increased CRABP in this study. However, the clinical experience with 9-cis retinoic acid,36 which does not bind to CRABP, may imply that CRABP is not the only cause of the ATRA resistance. We presume the more potent differentiation inducing activity of Am80 compared with ATRA has contributed the efficacy at least in some of our patients. In about 40% patients who did not respond to the Am80 therapy, further genetic mutations such as a point mutation of RAR-α may have occurred.
Because Am80 has little affinity to RAR-γ, the adverse effects related to this receptor would expectedly be less than those of ATRA. In fact, most patients as well as their attending physician stated that the cutaneous adverse events such as cheilitis and xerosis are less than those they had experienced during the previous ATRA therapy. However, the adverse events related to RAR-α and RAR-β would not theoretically be less, and we should be careful of such events as RA syndrome.
In this study we only treated patients who had less than 1 × 109/L blasts and promyelocytes in the PB to evaluate the efficacy of Am80 alone. This treatment protocol derived from our previous experience with ATRA, in which patients with high initial peripheral blast and promyelocyte counts often developed rapid hyperleukocytosis and required concomitant chemotherapy.4 Therefore, the low incidence of hyperleukocytosis in this Am80 therapy may have come from this eligibility criterion. Relapsed patients with APL generally have low leukemia burden due to early detection of leukemia relapse. Therefore, if we use this retinoid in newly diagnosed patients with APL, we may observe more hyperleukocytosis and RA syndrome, and may need concomitant chemotherapy in many patients.
Am80 will deserve further clinical trials in APL especially in combination with chemotherapy. Furthermore, a prospective randomized comparison between Am80 and ATRA, including a pharmacokinetic study, should be conducted both in relapsed and newly diagnosed patients with APL to clarify the therapeutic advantage of Am80.
ACKNOWLEDGMENT
We express our sincere gratitude to Dr Koichi Shudo (University of Tokyo Faculty of Pharmaceutical Sciences) for providing us Am80, and to Drs Masao Ino (Fujita-Gakuen Health University), Kazushige Yamada (Showa University School of Medicine), Yuji Ata (Okayama-Konan Hospital), Satoshi Miwa (Mie University School of Medicine), Masahiro Onoda (Narita Red-Cross Hospital), and Hisashi Fukutani (Okazaki City Hospital) for treating the patients in this study.
Supported in part by Grants-in-Aid of the Ministry of Education and Culture (No. 06266106, No. 07266106, No. 08266106) and the Ministry of Health and Welfare (No. 7-28).
Address reprint requests to Ryuzo Ohno, MD, Department of Medicine III, Hamamatsu University School of Medicine, 3600 Handa-cho, Hamamatsu 431-31, Japan.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal