To the Editor:
Although the French-American-British (FAB) classification1 has enabled the natural history of myelodysplastic syndromes (MDS) to be clarified, it has limitations as a prognostic parameter owing to the great variability in survival within each FAB subtype, especially refractory anemia (RA) and RA with ring sideroblasts (RARS). To obtain a better prognostic characterization of individual MDS patients, different scoring systems have been proposed,2-7 but imprecision persists with these analyses. In a recent issue of Blood, Greenberg et al8 described an International Prognostic Scoring System (IPSS) for MDS that was generated during an International MDS Risk Analysis Workshop. This system takes into account the number of cytopenias, bone marrow blast percentage, and refined cytogenetic characterization. In the investigators' experience, it provides an improved method for predicting survival and acute leukemia evolution with respect to the FAB, Sanz, and Morel categorization methods.
This publication prompted us to apply the new scoring system to MDS patients observed in our institution over the last 10 years and to compare its predictive value with that of the FAB classification and five previously published scoring systems.
The records of patients observed between 1986 and 1995 were examined: 143 cases of primary MDS not receiving intensive chemotherapy were found and the scoring systems of Mufti et al,2 Sanz et al,3 Goasguen et al,4 Morra et al,5 and Morel et al,7 in addition to the IPSS, were applied on the basis of data at diagnosis. According to the FAB classification, 52 patients had RA, 14 had RARS, 37 had RA with excess of blast cells (RAEB), 32 had RAEB in transformation (RAEB-t), and 8 had chronic myelomonocytic leukemia (CMML). Application of the Mufti, Sanz, Goasguen, and Morra scoring systems was possible in all cases, whereas IPSS and the Morel scoring systems were applied to 98 subjects only, because karyotype at diagnosis was not available for 45 subjects. This situation derived from a lack of evaluable mitoses in 15 cases and from the fact that cytogenetic investigation was not performed at diagnosis in 30 other patients. This latter phenomenon is not surprising, because chromosomal studies require specialized laboratories and are not always readily available everywhere; for example, in our institution, the cytogenetic laboratory is not operative on weekends and for 1 month during the summer.
Freedom from leukemia evolution and survival time were calculated using Kaplan-Meier curves.
Table 1 compares the effectiveness of the prognostic systems in the 95 patients with cytogenetic characterization at diagnosis; similar results were obtained when the scoring systems not requiring chromosomal mapping were applied to all 143 patients. Our results show that all prognostic systems gave similar results in the identification of patients with very short survival time and a high propension to acute leukemia transformation, whereas IPSS worked better in the categorization of subjects with intermediate risk. However, the IPSS was not satisfactory in the identification of patients with very long survival, in which the scoring systems of Morel, Sanz, and Goasguen and the FAB classification gave better results. The FAB classification and the Sanz and Goasguen systems offered the additional advantage in our study of MDS cases of allowing prognostic categorization of all patients, because they do not require cytogenetic studies.
Acute Leukemia Evolution and Survival Time of MDS Patients Within Subgroups Identified by Different Scoring Systems and the FAB Classification
| . | Risk Category . | ||||||
|---|---|---|---|---|---|---|---|
| . | Low . | Intermediate . | High . | . | . | ||
| . | . | . | . | . | . | . | . |
| A. Median survival (mo) | |||||||
| Prognostic system | |||||||
| Mufti | 32.7 | 17.6 | 11.9 | ||||
| Sanz | 64.3 | 14.4 | 11.9 | ||||
| Goasquen | 50.1 | 32.7 | 11.9 | 15.1 | |||
| Morra | 39.6 | 12.3 | 15.7 | 11.9 | |||
| Morel | 62.3 | 16.8 | 12.4 | ||||
| IPSS | 40.6 | 25.8 | 14.9 | 10.4 | |||
| FAB | 52.1 | 17.1 | 10.5 | ||||
| B. 25% acute leukemia evolution (mo) | |||||||
| Prognostic system | |||||||
| Mufti | NR | 8.3 | 6.2 | ||||
| Sanz | NR | 9.5 | 4.2 | ||||
| Goasguen | NR | 23.6 | 6.4 | 8.9 | |||
| Morra | 18.5 | 7.0 | 10.6 | 5.0 | |||
| Morel | NR | 8.8 | 6.0 | ||||
| IPSS | NR | 17.7 | 8.6 | 5.0 | |||
| FAB | NR | 9.2 | 4.7 | ||||
| . | Risk Category . | ||||||
|---|---|---|---|---|---|---|---|
| . | Low . | Intermediate . | High . | . | . | ||
| . | . | . | . | . | . | . | . |
| A. Median survival (mo) | |||||||
| Prognostic system | |||||||
| Mufti | 32.7 | 17.6 | 11.9 | ||||
| Sanz | 64.3 | 14.4 | 11.9 | ||||
| Goasquen | 50.1 | 32.7 | 11.9 | 15.1 | |||
| Morra | 39.6 | 12.3 | 15.7 | 11.9 | |||
| Morel | 62.3 | 16.8 | 12.4 | ||||
| IPSS | 40.6 | 25.8 | 14.9 | 10.4 | |||
| FAB | 52.1 | 17.1 | 10.5 | ||||
| B. 25% acute leukemia evolution (mo) | |||||||
| Prognostic system | |||||||
| Mufti | NR | 8.3 | 6.2 | ||||
| Sanz | NR | 9.5 | 4.2 | ||||
| Goasguen | NR | 23.6 | 6.4 | 8.9 | |||
| Morra | 18.5 | 7.0 | 10.6 | 5.0 | |||
| Morel | NR | 8.8 | 6.0 | ||||
| IPSS | NR | 17.7 | 8.6 | 5.0 | |||
| FAB | NR | 9.2 | 4.7 | ||||
For the FAB classification: low risk, RA + RARS; intermediate risk RAEB; high risk, RAEB-t + CMML.
Abbreviation: NR, not reached.
In conclusion, our experience confirms that the IPSS is effective in separating MDS patients into four groups with different life expectancies and tendencies to leukemia evolution. However, it was inferior to some of the older prognostic systems and to the FAB classification in the identification of very long survivors. Therefore, although the IPSS represents progress in the prognostic classification of intermediate-risk patients, it is not fully satisfactory and further investigation is required to devise better staging systems for proper risk-based therapeutic choices.
Response
Balduini et al have retrospectively examined clinical outcomes of myelodysplastic syndrome (MDS) patients from their institution using a number of prognostic systems for MDS, including our recently published International Prognostic Scoring System (IPSS). Of the 143 patients they evaluated, only two thirds had marrow cytogenetics determined, for which (in their Table 1) they show survival and AML evolution times. Their interpretation of their data is that all the systems they used gave similar results for poor (high) risk patients and the IPSS gave “better” results for intermediate patients, whereas a number of other systems gave “better” results for low-risk patients with relatively longer survivals.
As we reported in our analyses using the proportional hazards regression model, the predictive power for the IPSS was compared with that for the FAB, Spanish, and Lille systems.1-1 In these comparisons, the IPSS effectively discriminated between the defined subgroups of these other categorization systems (p 2083) and had statistically greater discriminating power compared with that of the other methods. From the information sent by Balduini et al, it is unclear what they mean by “better” results with their use of certain prognostic systems. For such a statement to be made, statistical analysis and careful examination of the comparative survival curves are required, not merely stating median survival times.
As we also indicated in our report, another critical variable for analyzing clinical outcome is the patient's age.1-1 The relative age distribution of patients has major impact on survival of the evaluated group, with younger patients having improved survival, particularly in low and intermediate-1 (Int-1) risk individuals. It would thus be helpful to have been informed of this feature of Balduini's patients to determine whether this affected their low-risk patients' outcomes. Similarly, other selective features (eg, FAB subtypes) of the 95 patients they analyzed compared with their entire group would also be useful to know.
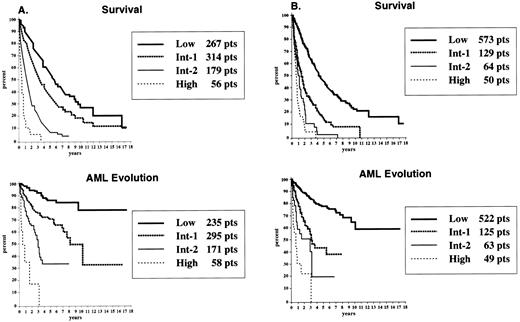
Balduini et al commented on their finding that several of the systems they used that had “better” results for low-risk patients had the advantage of not requiring cytogenetic analyses (ie, FAB, Spanish, and Goasguen et al). However, our study1-1 and those of others1-2,1-3 clearly showed the importance of cytogenetic subtypes as a major variable in determining clinical outcome, particularly in the low and intermediate risk categories.1-1 As seen in the survival curves of our workshop patients assessed with and without cytogenetic evaluation (Fig 1-1), the percentage of patients within the high-risk subgroups was similar when using the “complete” IPSS (7% of patients) versus the “partial” model (ie, without cytogenetics; 6%), driven mainly by marrow blast percentage and associated cytopenias. However, much less discriminating power for the intermediate and low-risk patients was demonstrated when cytogenetics were omitted from the classification method. As shown in Fig 1-1, due to cytogenetics a redistribution of patients occurred from the low into the Int-1 and Int-2 risk groups: low, 33% (“complete” IPSS) from 70% (“partial”); Int-1, 38% from 16%; Int-2, 22% from 8%. Thus, cytogenetic features contributed substantially to patients' Intermediate-1 and -2 categorizations, the patients generally most difficult to classify. This improved separation of patients into prognostically more accurate subgroups by the IPSS was also demonstrated by statistical analyses showing increased log-rank χ2 values for the model with cytogenetics (in addition to marrow blasts and number of cytopenias) included. These proportions of patients, survival curves, and associated statistical values are not provided by Balduini, but would be helpful to know. Although cost and technical facility make cytogenetic evaluation nonroutine, we believe our data indicate the value of cytogenetics and the IPSS for improved decision-making in this complex disease.
Survival (top) and freedom from AML evolution (bottom) of MDS patients related to their IPSS risk groups, with (A) and without (B) cytogenetics included in the classification system. The curves for (A) have been reprinted with permission from Greenberg et al.1-1
Survival (top) and freedom from AML evolution (bottom) of MDS patients related to their IPSS risk groups, with (A) and without (B) cytogenetics included in the classification system. The curves for (A) have been reprinted with permission from Greenberg et al.1-1

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal