Abstract
In an attempt to restore immune competence to 12 human immunodeficiency virus-1 (HIV-1)–infected patients, lymphocytes from their HIV-1–uninfected identical twin siblings were cultured in medium supplemented with 5% fetal calf serum (FCS), anti-CD3 antibody, and interleukin-2 (100 IU/mL) for 10 days and then infused into the patients. After multiple infusions, at 6- to 8-week intervals, half of the patients developed arthus-like reactions within 4 to 12 hours of infusion consisting of fever <39°C, hypotension, rigors, arthralgias, myalgias, headache, and/or malaise. Preinfusion and postinfusion serum samples were evaluated for the presence of antibodies to FCS using double immunodiffusion. All preinfusion serum samples were negative by this method while 8 of the 12 patients developed antibodies to a single component of FCS after two or more infusions of lymphocytes cultured in FCS-supplemented medium. Prick skin testing to standardized beef extract was negative in all patients. There was a correlation between initial CD4 level and the development of antibodies to FCS (median initial CD4 count in FCS antibody positive patients = 362.0/μL v median initial CD4 count of nonresponders = 135.0/μL). There was no correlation with response to recall antigens in delayed-type hypersensitivity testing. We conclude that selected patients were sensitized to a single component of FCS carried on donor lymphocytes, despite thorough washing of the cells before infusion. The development of antibodies to FCS indicates that immune complex formation could have occurred after the cell infusions, resulting in the arthus-like reactions. These observations suggest that the therapeutic use of human lymphocytes cultured in FCS may expose the recipient to immunogenic substances with possible clinical sequelae.
THE BASIC immunologic defect in the human immunodeficiency virus (HIV)-infected patient is a progressive loss of CD4 T lymphocytes leaving the patient susceptible to opportunistic infections normally controlled by cell-mediated immunity. Over the past 12 years, an inverse relationship between the total CD4 count and the severity of opportunistic sequelae has been established.1-4 Multiple methods including antiretroviral and intravenous (IV) cytokine therapies have been used in an attempt to prevent the inevitable decrease in the CD4 lymphocyte count and resultant immunosuppression seen with HIV infection. A novel therapy utilizes the technology of lymphocyte transfer to attempt direct maintenance of immune competent T lymphocytes through the provision of syngeneic lymphocytes.
Adoptive cell therapy (ie, lymphocyte transfer) has been investigated as an approach to therapy of multiple disorders including malignancy, immune deficiencies, and certain infectious diseases.5-10 Limited success has been achieved to date; however, with the advent of genetic manipulation of cells, strategies for ex vivo cell expansion and activation are becoming more important. The expansion of lymphocytes ex vivo requires the use of growth factors and other stimulants. For CD4 cells in particular, both well-characterized (interleukin-2 [IL-2] and anti-CD3)5,11 and poorly characterized (fetal calf serum [FCS])12 reagents appear to be required.
In a recent clinical trial, lymphocyte transfer involving 12 HIV-1–infected twins using lymphocytes prepared from their HIV-1–uninfected identical twin siblings13 has been associated with certain clinical side effects, the most significant of which were manifestations of an arthus-like reaction consisting variously of prolonged fever, orthostasis, headache, myalgias, arthralgias, chest tightness, malaise, fatigue, and rigors. We evaluated these reactions, previously undescribed with lymphocyte transfers, with a double-immunodiffusion assay and showed the presence of antibodies to FCS in two thirds of the patients infused with lymphocytes cultured in medium supplemented with 5% FCS.
MATERIALS AND METHODS
Patients.Twelve pairs of identical twins discordant for HIV-1 infection were enrolled in a study of syngeneic lymphocyte transfer at the National Institute of Allergy and Infectious Diseases (NIAID). The study was approved by the NIAID Institutional Review Board.
Preparation of cells.The HIV-1–uninfected identical twin sibling donors underwent lymphapheresis 10 days before transfer of donor lymphocytes to the HIV-1–infected twin. The collected cells were cultured in AIM-V serum free medium (GIBCO-BRL, Life Technologies, Grand Island, NY) supplemented with 5% FCS (Sigma, St Louis, MO), anti-CD3 antibody (Ortho, Raritan, NJ; 10 ng/mL), recombinant IL-2 (Chiron Corp, Emeryville, CA; 100 IU/mL). After 10 days of ex vivo expansion, the donor lymphocytes were washed 10 times in normal saline solution and then infused into the HIV-1–infected recipient. These infusions were repeated at 6- to 8-week intervals for a total of three administrations in seven patients and four administrations in two patients. Five patients had one additional preparation of donor lymphocytes cultured in autologous or human serum without FCS. One patient had an additional preparation of donor lymphocytes cultured in the standard medium with FCS for 7 days followed by washing the cells and culturing them in medium with human plasma for the final 72 hours.
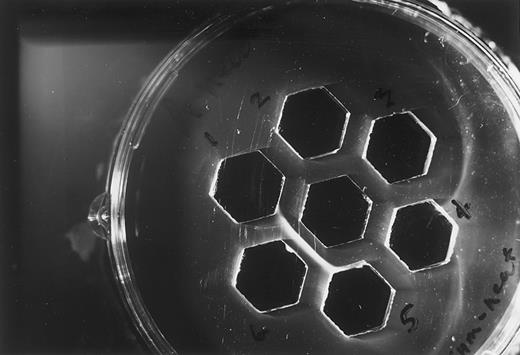
Evaluation for antibody to FCS.Double-immunodiffusion testing (Nova Gel T Plates; INOVA Diagnostics, Inc, San Diego, CA) for antibodies to FCS in the serum of patients given the syngeneic lymphocyte transfer was performed and compared with matched control preinfusion sera. Serum specimens were obtained from the patients 1 to 7 days before the initiation of the study and 2 weeks after each infusion. Fifty microliters of FCS, obtained from the same lot as that used to supplement the AIM-V medium for cell culture, was placed in the center well of the gel plate at 1:1, 1:5, and 1:10 dilutions. Preinfusion and postinfusion specimens were placed in the surrounding wells and the plates were read at 48 and 72 hours. A positive result was based on the presence of a discreet linear precipitin line visible in the gel between the center well containing FCS and the sample well by indirect incandescent lighting (Fig 1). Double-immunodiffusion testing was performed on selected patients' sera positive for the development of FCS antibodies using purified bovine serum albumin (Sigma) as the antigen. Additionally, all positive patient sera were compared for identity of the precipitin reaction using double immunodiffusion with FCS as the antigen.
Representative double immunodiffusion for three patients receiving syngeneic lymphocytes cultured with FCS. Center well, undiluted FCS; well 1, patient 12 preinfusion serum; well 2, patient 12 serum after first infusion; well 3, patient 2 preinfusion serum; well 4, patient 2 serum after first infusion; well 5, patient 8 preinfusion serum; well 6, patient 8 serum after the fourth infusion.
Representative double immunodiffusion for three patients receiving syngeneic lymphocytes cultured with FCS. Center well, undiluted FCS; well 1, patient 12 preinfusion serum; well 2, patient 12 serum after first infusion; well 3, patient 2 preinfusion serum; well 4, patient 2 serum after first infusion; well 5, patient 8 preinfusion serum; well 6, patient 8 serum after the fourth infusion.
Bovine skin testing.Prick skin testing with 1:1 dilution of beef antigen extract (Miles Pharmaceutical, Spokane, WA) was done with 1/20 wt/vol (weight per volume).
Delayed-type hypersensitivity (DTH).DTH responses were performed by using the Multitest CMI intradermal injection method (Connaught Laboratories, Inc, Swiftwater, PA) and the Tetanus Toxoid fluid purified Ultrafined (0.1 mL intradermal injection; Wyeth Laboratories, Inc, Marietta, PA). Negative results on both tests were interpreted as a negative response whereas positive results on either test were interpreted as a positive response.
RESULTS
Syngeneic lymphocytes cultured in FCS induced arthus-like reactions and positive antibodies to FCS.Eleven of 12 patients (92%) receiving IV syngeneic lymphocytes grown in FCS developed symptoms consisting of one or more of the following: fever, headache, orthostasis, arthralgias, myalgias, fatigue, rigors, and chest tightness. Six of the 12 patients developed specific arthus-like symptoms defined as temperature >39°C and/or orthostasis accompanied by one of the following: rigors, chills, chest tightness, arthralgias, or myalgias (Table 1). In general, symptoms worsened with subsequent infusions and all the patients with arthus-like symptoms developed positive double-immunodiffusion tests for antibodies to FCS (Fig 1). Overall, 8 of the 12 patients developed antibodies to FCS. The two patients who developed antibodies to FCS but did not demonstrate arthus-like symptoms had received antipyretic and antihistamine therapy during each infusion after the first infusion (Table 2).
Clinical and Immunologic Evaluation of HIV Patients Exposed to Syngeneic Lymphocytes Cultured in FCS
| Patient . | No. of FCS Exposures . | FCS Double Immunodiffusion . | Arthus-Like Symptoms* . | Bovine Skin Test . | Initial CD4 Count/μL . | DTH Response . |
|---|---|---|---|---|---|---|
| 1 | 3 | − | − | 54 | − | |
| 2 | 2 | − | − | − | 73 | − |
| 3 | 3 | + | + | − | 116 | + |
| 4 | 3 | + | + | 135 | − | |
| 5 | 3 | − | − | − | 197 | + |
| 6 | 2 | + | + | − | 224 | − |
| 7 | 2 | − | − | − | 230 | + |
| 8 | 4 | + | + | − | 281 | + |
| 9 | 3 | + | − | 444 | + | |
| 10 | 3 | + | + | − | 469 | + |
| 11 | 4 | + | + | − | 493 | − |
| 12 | 2 | + | − | − | 595 | + |
| Patient . | No. of FCS Exposures . | FCS Double Immunodiffusion . | Arthus-Like Symptoms* . | Bovine Skin Test . | Initial CD4 Count/μL . | DTH Response . |
|---|---|---|---|---|---|---|
| 1 | 3 | − | − | 54 | − | |
| 2 | 2 | − | − | − | 73 | − |
| 3 | 3 | + | + | − | 116 | + |
| 4 | 3 | + | + | 135 | − | |
| 5 | 3 | − | − | − | 197 | + |
| 6 | 2 | + | + | − | 224 | − |
| 7 | 2 | − | − | − | 230 | + |
| 8 | 4 | + | + | − | 281 | + |
| 9 | 3 | + | − | 444 | + | |
| 10 | 3 | + | + | − | 469 | + |
| 11 | 4 | + | + | − | 493 | − |
| 12 | 2 | + | − | − | 595 | + |
Arthus-like symptoms defined as temperature >39°C and/or orthostasis accompanied by one of the following: rigors, chills, chest tightness, arthralgias, or myalgias.
Double Immunodiffusion for FCS Antibodies and Arthus-Like Symptoms After Each FCS Exposure
| Patient . | Infusion . | |||
|---|---|---|---|---|
| . | 1 . | 2 . | 3 . | 4 . |
| 1 | −* | −* | −* | |
| 2 | − | −* | ||
| 3 | ND | +† | ||
| 4 | − | −† | +*† | |
| 5 | − | −* | −* | |
| 6 | − | +† | ||
| 7 | − | − | ||
| 8 | − | −* | +* | +† |
| 9 | −* | −* | +* | |
| 10 | − | + | +† | |
| 11 | −* | −* | + | +† |
| 12 | − | +* | ||
| Patient . | Infusion . | |||
|---|---|---|---|---|
| . | 1 . | 2 . | 3 . | 4 . |
| 1 | −* | −* | −* | |
| 2 | − | −* | ||
| 3 | ND | +† | ||
| 4 | − | −† | +*† | |
| 5 | − | −* | −* | |
| 6 | − | +† | ||
| 7 | − | − | ||
| 8 | − | −* | +* | +† |
| 9 | −* | −* | +* | |
| 10 | − | + | +† | |
| 11 | −* | −* | + | +† |
| 12 | − | +* | ||
Abbreviation: ND, not determined.
Premedicated with antihistamines and/or antipyretics.
Infusions with arthus-like symptoms (defined as temperature >39°C and/or orthostasis accompanied by one of the following: rigors, chills, chest tightness, arthralgias, or myalgias).
None of the 11 patients' sera which were evaluated after the first infusion were positive by immunodiffusion, but one third of the sera (4 of 12) were positive after the second infusion (Table 2). Seven patients underwent a third infusion with lymphocytes that had been cultured in FCS. Of these, 1 had previously developed antibodies to FCS and an additional 4 developed FCS antibodies after this third infusion. Thus, only 2 of the 7 patients receiving three transfusions with lymphocytes cultured in FCS containing medium failed to develop antibodies (Table 2), resulting in a cumulative 80% seroconversion after the third exposure to FCS. The other 2 patients who failed to develop antibodies to FCS had only two infusions with lymphocytes cultured in FCS.
The antibodies to FCS are against a common antigen that is not bovine serum albumin (BSA).The serum of each patient which was shown to have an antibody to FCS was tested by double immunodiffusion with each of the other positive sera using FCS as the antigen to evaluate for possible identity. All precipitin lines demonstrated identity indicating a single common antigen (data not shown). Selected patients' sera reactive to FCS were tested against purified BSA and no precipitins were found (data not shown), showing that at least this major constituent of FCS was not responsible for anti-FCS antibodies observed in these patients.
Absolute peripheral CD4 T-cell levels correlate with the development of antibodies to FCS.The eight patients who were positive for antibody by double immunodiffusion had a median CD4 count of 362.0/μL which was more than 2.5 times greater than those without demonstrable antibody (median = 135.0/μL). Of the four patients with negative double-immunodiffusion tests for antibody to FCS, all had absolute CD4 T-cell levels of <250/μL at the initial infusion (Table 1). Two of these patients received only two infusions of cells cultured in FCS. The two patients who developed antibodies to FCS after receiving only two lymphocyte infusions had absolute total CD4 T-cell counts of 224 and 595/μL.
Loss of DTH responses did not correlate with development of an antibody response to FCS.Two of the patients who failed to develop antibody responses to FCS were unable to mount DTH responses to recall antigens. However, three of the eight persons who developed antibodies to FCS were also found to be anergic by DTH testing, suggesting little correlation between the development of antibodies to FCS and DTH response.
No IgE antibody to standardized beef extract was shown.Infusion of lymphocytes cultured in FCS did not likely elicit an IgE-mediated anaphylactic reaction because skin prick test to standardized beef antigen was negative in nine of the nine patients tested subsequent to lymphocyte infusions.
Lymphocytes cultured in human plasma did not cause arthus-like reactions.None of the six patients who received lymphocytes cultured in human plasma showed signs or symptoms of arthus-like reactions upon transfer of the lymphocytes. One of the six did develop headache and arthralgias, but these symptoms were milder than those observed previously in this patient and did not include temperature elevation. The number of cells transferred after ex vivo expansion without FCS was substantially lower (range: 2.5 × 109 to 1.0 × 1010) than the numbers administered after culture with FCS (range: 2.1 × 1010 to 6.8 × 1010), which may have contributed to the absence of associated arthus-like symptoms.
DISCUSSION
Anaphylactic reactions to FCS in patients treated with cultured white blood cells have been previously reported.14 We now report a non–IgE-mediated reaction to FCS in HIV-infected patients after multiple transfers of syngeneic lymphocytes cultured in FCS, consistent with a type III hypersensitivity reaction.
The role of FCS in the induction of the clinical symptoms in these patients is suggested by (1) the correlation between the development of symptoms and the appearance of antibodies to FCS, and (2) the absence of significant symptoms when cells were cultured in AB human serum instead of FCS. We considered the possibility of incidental infusion of IL-2 from the activated lymphocyte preparation, but IL-2 in the washed preparation just before infusion was undetectable by enzyme-linked immunosorbent assay. In addition, there was no significant detection of IL-6, IL-1β, and tumor necrosis factor-α in the washed preparation.
Over the past several decades, multiple immunomodulatory effects of FCS have been demonstrated, including natural killer cell activation,15 induction of major histocompatibility complex–unrestricted cell-mediated cytotoxicity,16,17 induction of lymphokine secretion, and polyclonal B-cell activation.18 It is likely that many, if not all, of these effects may have played a role in the generation of these patients' responses. In 1991, Reisser and Michel19 described the adsorption of components of fetal bovine serum to rat colon cancer cells which altered the immune response to these cells when injected into syngeneic mice. Similarly, the demonstration of antibody to FCS by immunodiffusion in our patients after infusions with cultured lymphocytes suggests that the washing procedures before infusion were inadequate to remove foreign FCS proteins from those lymphocytes. The possibility also exists that the transferred syngeneic lymphocyte may play an active role in sensitizing the patient to FCS rather than merely serving as a passive vehicle for the foreign antigen.
Antibody to a neoantigen expressed on human cell lines cultured in fetal bovine serum has been demonstrated in the serum of approximately 50% of normal individuals.20 If such a natural antibody to FCS does exist in our patients, the titer was too low for detection by immunodiffusion before the cell infusions. The presence of clinical symptoms of an arthus-like reaction that worsened on repeated administration of cells suggests a boosting effect to one or more components of FCS on repeat exposure. However, one cannot rule out the augmentation of the titer of FCS antibody in an anamnestic fashion resulting from naturally occurring antibody or previous low-level sensitization from bovine product ingestion.
Efforts to characterize the specificity of the patients' antibodies ruled out reactivity against BSA, the major protein constituent of FCS. However, we did demonstrate by double immunodiffusion that all patients' antibodies react with the same antigen in the FCS. This suggests that there is a dominant immunogenic substance present on lymphocytes cultured in FCS capable of eliciting a humoral immune response following repeated exposure.
Although 4 of the 12 patients did not develop detectable antibodies to FCS with infusions, these four patients had markedly lower CD4 T-cell counts, suggesting that their immunologic compromise had progressed to an inability to competently generate antibody to the infusion of foreign proteins. Thus, it appears that the development of both arthus-like symptoms and antibodies to FCS in these patients was dependent on repeated exposures to FCS in an individual without severe cell-mediated immune dysfunction.
Sensitization to foreign proteins from lymphocytes cultured ex vivo may be a treatment-limiting phenomenon especially when the cellular source is syngeneic or autologous. With the increasing potential use of ex vivo cell preparations for therapeutic interventions, it is critical to identify the various immunologic reactions that may be induced by such therapy and modify them accordingly. Our results indicate the importance of developing cell culture methods that are appropriate for human clinical trials and that do not rely on FCS-containing media. As shown in the present study, the mere substitution of human AB serum severely limits the capacity of the T cells to undergo expansion in response to anti-CD3 and recombinant IL-2. Therefore, the challenge will be to find a serum additive(s) that will permit adequate expansion of lymphocytes without also acting as a potent immunogen.
Supported by the National Institute of Allergy and Infectious Diseases and Warren Magnuson Clinical Center, National Institutes of Health.
Address reprint requests to Thomas A. Selvaggi, MD, Room 2C410, 10 Center Dr, MSC 1508, Bethesda, MD 20892-1508.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal