In this issue of Blood, Bhatla and colleagues report on the phase 2 Delphinus study that evaluated daratumumab as part of combination therapy in pediatric and young adult patients with relapsed/refractory (R/R) acute lymphoblastic leukemia (ALL) and show efficacy in the T-cell cohort.1 The study included pediatric patients with R/R B-cell ALL (B-ALL) for second and further salvage treatments and pediatric and young adult patients with R/R T-cell ALL (T-ALL)/T-lymphoblastic lymphoma (LBL) for first salvage therapy. The primary end point of the study was the rates of complete remission (CR) after 1 cycle of therapy in the B-ALL cohort and 2 cycles of therapy in T-ALL/LBL cohort. The efficacy results of interest focus on the T-ALL/LBL cohort, while the B-ALL cohort had to be closed early in view of futility.
Development of targeted drugs in T-ALL/LBL has lagged behind that of B-ALL, and outcomes in R/R T-ALL/LBL remain dismal, with median overall survival of 6 to 9 months.2,3 In the absence of targeted therapies and a chimeric antigen receptor T-cell (CART) therapy, most patients with R/R T-ALL/LBL receive agents like nelarabine, often in combination with other chemotherapeutic agents for salvage therapy.4,5 Remission rates of around 50% to 60% are obtained in first salvage treatment and around 20% to 30% in further salvage treatments. Additionally, the durability of second and subsequent remissions remains short, often precluding a consolidative allogeneic hematopoietic stem cell transplantation (HSCT), the only curative therapy in these settings.
CD38 is highly expressed in T lymphoblasts, and targeting CD38 has been shown to be effective in preclinical studies of R/R T-ALL.6,7 CD38 is an ectoenzyme that is involved in T-cell activation and in modulating proliferation.8 Daratumumab is a naked immunoglobulin G1-κ monoclonal antibody that targets CD38 and causes cell death primarily through complement-dependent cytotoxicity and antibody-dependent cellular phagocytosis and is approved for use in frontline and R/R multiple myeloma.9 In the Delphinus study daratumumab was evaluated in combination with vincristine and prednisone in R/R B-ALL or doxorubicin, vincristine, prednisone, and pegylated asparaginase in R/R T-ALL/LBL along with intrathecal methotrexate.
Among the 7 patients with B-ALL, none achieved CR, and this arm was terminated. Thirty-nine patients with T-ALL/LBL (pediatric T-ALL = 24, young adult T-ALL = 5, pediatric or young adult T-LBL = 10) were treated. Eight patients (20%) had concomitant central nervous system (CNS) disease at the study enrollment. The best overall response rate was 74% with a CR rate of 49%. The CR rates were higher in patients with T-ALL (52%) compared with patients with T-LBL (40%). Twelve of the 29 patients with T-ALL (41% of all patients and 50% of responding patients) achieved measurable residual disease (MRD)-negative status. More importantly, 24 patients (61%) received subsequent consolidation with an HSCT (21 of 29 patients with T-ALL and 3 of 10 patients with T-LBL), the goal of such a salvage regimen in these patients. The achievement of good MRD rates in the T-ALL cohort with the study regimen is of relevance, as this remains the ideal time to consider an HSCT.
Survival outcomes (event-free survival and overall survival) were superior in the T-ALL cohort compared with the T-LBL cohort. More patients in the young adult T-ALL (60%) and the T-LBL (50%) groups had primary refractory disease compared with the pediatric T-ALL group (25%); this accounts for the longer median time from end of prior systemic therapy to salvage therapy for the pediatric T-ALL cohort (12.5 months) compared with <1 month for the young adult T-ALL and LBL cohorts. Longer first remission is associated with superior outcomes after salvage therapy, and this might have led to the better outcomes in the pediatric T-ALL cohort. Certainly, different disease biology of T-ALL and T-LBL could also be dictating the inferior outcomes in the latter.
The authors show that the mean baseline expression of CD38 was associated with postdaratumumab response in the T-ALL/LBL cohort, and there was a progressive reduction in CD38 expression with therapy. Although such a reduction was also seen in the small B-ALL cohort, no one had a response. Furthermore, the authors show a cumulative increase in daratumumab serum levels but with no significant CNS penetration. Thus, the efficacy of daratumumab in patients with CNS leukemia remains questionable. A sizeable proportion of patients with T-ALL and extramedullary disease had an overall response, though granular details of response among patients who had CNS disease in the T-ALL/LBL cohort would have been interesting to see. The regimen appeared well tolerated with 2 events of grade 3 infusion reaction, and no cautionary safety signal was noted, beyond what would be expected in such salvage settings.
The Delphinus study adds evidence toward the efficacy and feasibility of daratumumab in R/R T-ALL/LBL, warranting further evaluation of the drug in larger studies. Nelarabine is approved for R/R T-ALL; combining active agents is needed in earlier salvage treatments where the possibilities of attaining a deep and durable remission is higher and increases the probability of a successful consolidative HSCT, rather than sequential use of these drugs at salvage attempts. Also, using MRD-directed therapy with daratumumab as part of frontline therapy in T-ALL/LBL is an avenue that needs to be prospectively evaluated. Combination of chemotherapy with nelarabine, pegylated asparaginase, and MRD-based venetoclax dosing has shown promising outcomes in the frontline setting for adults with T-ALL/LBL, including in the early T-cell precursor phenotypes.10
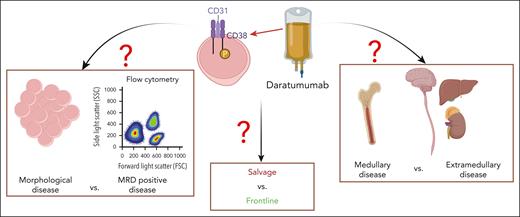
The small patient number is a particular limitation of the study. The assessment of the drug in R/R B-ALL was futile. Established salvage options in R/R B-ALL like inotuzumab ozogamicin, blinatumomab, and anti-CD-19 CART therapy needs to be used first. However, it is still important for drug development in R/R B-ALL as B-cell-targeted agents are now often used in earlier therapy lines and relapse after exposure to these agents remain a very challenging situation. With the wide experience of daratumumab in multiple myeloma and with its established safety profile, the evidence from the Delphinus study certainly makes the drug an important treatment option in T-ALL/LBL. Choosing the right time points and disease setting for using daratumumab in T-ALL/LBL needs to be efficiently studied in randomized clinical trials (see figure).
Deciphering the ideal clinical setting for daratumumab use in T-cell ALL/LBL remains to be evaluated. Figure made in Biorender.com.
Deciphering the ideal clinical setting for daratumumab use in T-cell ALL/LBL remains to be evaluated. Figure made in Biorender.com.
Conflict-of-interest disclosure: E.J. received research grants from AbbVie, Adaptive Biotechnologies, Amgen, Pfizer, and Takeda and consultancy fees from AbbVie, Adaptive Biotechnologies, Amgen, Bristol Myers Squibb, Genentech, Incyte, Novartis, Pfizer, and Takeda. J.S. declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal