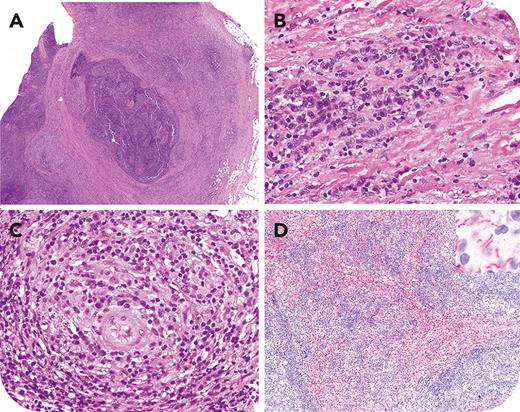
A 33-year-old man presented with a 1-month history of left groin swelling, with no other significant complaints. Imaging revealed prominent external iliac and inguinal lymphadenopathy. Biopsy showed matted lymph nodes with capsular fibrosis (panel A: hematoxylin and eosin [H&E] stain, 2× lens objective) and dense inflammatory infiltrate. Vascular proliferation with perivascular cuffing by plasma cells was noted (panels B-C: H&E stain, 50× lens objective). Larger caliber vessels showed features of obliterative arteritis and histocytic collections forming vague granulomas near the vessel wall. Stains for acid-fast bacilli and fungi were negative. Treponema pallidum immunohistochemical stain revealed numerous organisms (corkscrew morphology) in aggregates and distributed perivascularly (panel D: 10× lens objective, inset: 100× lens objective). Subsequently, the patient developed night sweats and a rash on his palms and soles. A reactive rapid plasma reagin test confirmed secondary syphilis (titer: 1:64).
Treatment with benzathine penicillin G for the patient and doxycycline for his partner was initiated. Although this constellation of histologic findings is not pathognomonic of syphilitic lymphadenitis, it is distinctive enough to suggest syphilis as a potential diagnosis. An immunohistopathologic diagnosis of syphilis enabled timely treatment, prevention of long-term sequelae, and reduced transmission risk.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal