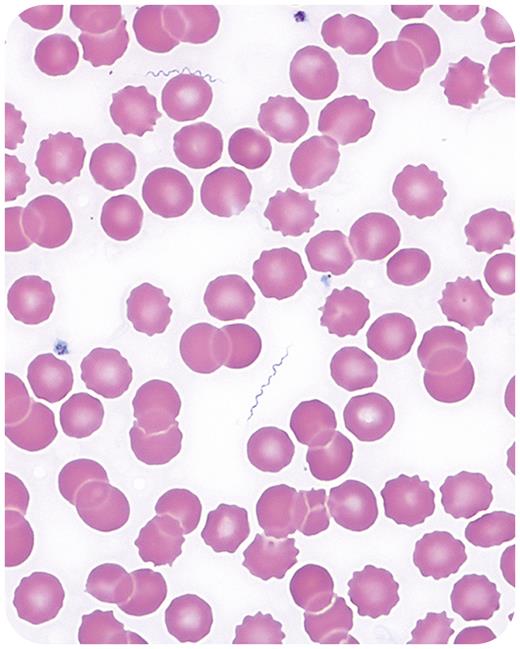
One day after returning home from a 5-week trip to Colorado, a 65-year-old woman came to the emergency department with a 3-day history of fever and altered mental status, described as flat affect with apathy and difficulty thinking through tasks. The patient recalled multiple insect bites of unclear source but denied any tick exposure during the trip. Laboratory results showed elevated inflammatory markers with procalcitonin of 2.26 ng/mL, elevated liver function tests with alanine transaminase 116 units/L and aspartate transaminase 106 units/L, and hyperbilirubinemia (2.2 mg/dL). Complete blood count showed thrombocytopenia (103 000/μL) and absolute lymphopenia (800/μL). Numerous spirochetes were identified on a peripheral blood smear (see figure; 100× objective). She was started on ceftriaxone and doxycycline for possible central nervous system involvement and showed rapid cognitive improvement with a reassuring lumbar puncture. Serum from the patient showed immunoglobulin G reactivity to Borrelia hermsii, and a blood sample sent for polymerase chain reaction detection confirmed the diagnosis of tick-borne relapsing fever.
Tick-borne relapsing fever is an endemic zoonosis in North America, caused by various Borrelia species and transmitted to humans by soft ticks with a rapid feeding pattern that goes unnoticed by most patients. Antigenic variation during the time of high replication is responsible for the relapsing pattern of febrile episodes. Although molecular testing allows for identification, a blood smear can provide inexpensive and rapid diagnostic information in this setting.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal