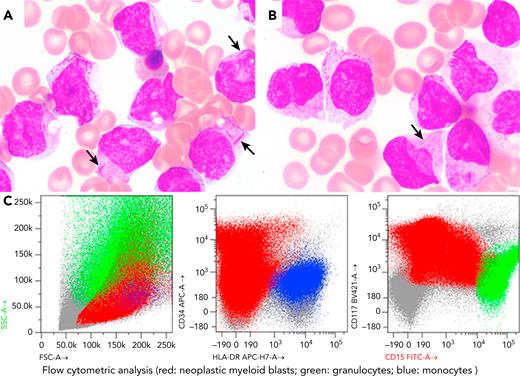
A 56-year-old woman was admitted for anemia (hemoglobin, 7.8 g/dL) and thrombocytopenia (platelets, 25 000/μL), which was concerning for acute myeloid leukemia (AML). The peripheral blood (PB) and bone marrow (BM) aspirate smears showed numerous hypergranular promyelocytes with Auer rods (panels A and B, black arrows; Wright-Giemsa stain on BM aspirate; 100× objective). Flow cytometric study on BM aspirate (panel C) demonstrated abundant promyelocytes (62%) with high side scatter (corroborating hypergranularity) and CD34partial+/human leukocyte antigen (HLA)-DRpredominantly−/CD15partial+/CD117+. There was a mild increase in D-dimer (2.31 μg/L; reference value, ≤0.59 μg/L). These findings were suspicious for acute promyelocytic leukemia (APL). The patient was initially treated with all-trans retinoic acid, but treatment was discontinued once fluorescence in situ hybridization studies indicated an NUP98 rearrangement but no evidence of PML::RARA or RARA rearrangement. Cytogenetics revealed an isolated 46,XX,t(7;11)(p15;p15), resulting in the NUP98::HOXA9 fusion that was confirmed by next-generation sequencing (NGS) (additional TET2 [p.Leu1229Arg and p.Gln635∗] detected). The patient was started on standard induction chemotherapy with the 7 + 3 regimen.
To our knowledge, this is the first case of NUP98::HOXA9 rearranged AML that morphologically and immunophenotypically resembles APL; notably, NUP98::RARA fusion has been recently reported in APL. This case highlights the importance of combining different techniques (PB/BM examination, flow cytometry, cytogenetics, and NGS) to identify driver lesions and select appropriate therapies.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal