In this issue of Blood, Tashakori et al1 elucidated the genomic and proteomic features of TP53-mutated acute myeloid leukemia (AML), a disease with a dismal prognosis that is currently spread across several AML disease categories.
TP53 mutation confers a poor prognosis for multiple neoplasms, and AML is no exception. TP53 mutation is considered in the adverse prognostic group of the 2017 ELN (European LeukemiaNet) Classification of AML,2 although recent data suggest that TP53-mutated AML confers a particularly poor prognosis compared with other ELN adverse cases, with a 2-year median overall survival of only 12.8% even when intensively treated.3 Moreover, the dismal effect of TP53 on patient outcome appears to transcend both blast count and disease ontogeny, with equally poor outcomes whether patients present as myelodysplastic syndrome (MDS) or AML, and whether the disease is therapy-related or clinically de novo.4 However, several nagging questions remain as to how to best categorize AML patients in which TP53 mutations are detected. Are all somatic TP53 mutations equally pathogenic? Does the variant allele frequency (VAF) of the mutation matter? Although mostly associated with complex karyotypes, do cases with noncomplex karyotypes differ in their behavior? Is the loss of the wild-type allele (located at chromosome 17p) required for mutated TP53 mutation to exert its effects, promoting genetic instability and an aggressive disease phenotype?
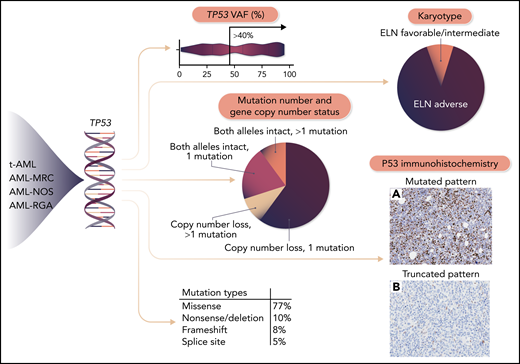
In a comprehensive analysis of 442 AML patients with mutated TP53, Takashori and colleagues have begun to answer these questions, shedding light on the heterogeneity of TP53-mutated AML and underscoring the importance of nuanced interpretation of individual TP53 mutations. The authors found a diverse spectrum of mutations in the gene, with missense mutations in the DNA-binding domain being most common, followed by nonsense, frameshift, deletion, and splice-site mutations (the latter also mainly distributed around the DNA binding domain). They found a wide range of TP53 mutation VAFs, which correlated only loosely with the bone marrow blast percentage, underscoring the fact that TP53 mutations are usually carried not only with the blasts but also in nonblast hematopoietic cells.5
Mutant p53 protein, largely by virtue of its resistance to degradation, accumulates in affected cells and can be detected by immunohistochemistry in bone biopsy sections.6 Tashakori and colleagues applied p53 immunohistochemistry to a series of 211 AML patients and confirmed that the staining pattern correlated very strongly with the presence of TP53 mutation. Using a digital image analysis algorithm, they arrived at an optimal cutoff of 7.2% strong p53-positive cells (or completely absent staining due to a truncated protein), achieving a positive predictive value of 93.75% and negative predictive value of 91.57% in their cohort. Unlike TP53 mutation analysis by next-generation sequencing (NGS), which typically has a turnaround time of 1 to 2 weeks, immunohistochemistry can usually be performed in 24 hours and thus has the potential to identify these ultra high-risk AML patients more rapidly than waiting for NGS results. Moreover, immunostaining revealed several discordant cases in which a TP53 mutation was overcalled on the initial NGS report, suggesting potential utility as an orthogonal method to confirm a biologically significant mutation.
The authors also examined factors influencing outcomes in their TP53-mutated AML cohort. As expected, an adverse (usually complex) karyotype was associated with shorter overall survival and was seen in the vast majority of patients. In concordance with the data for MDS, multihit TP53 mutation (due to copy number loss or multiple mutations) was also associated with shorter survival. An important aspect is whether an intact wild-type TP53 allele can partly abrogate the effect of a single mutated TP53 gene. In MDS, single (monoallelic) TP53-mutated cases exhibit biologically distinct features and a more favorable prognosis than cases exhibiting loss of the wild-type allele (“multihit”); the latter can occur due to deletion of the 17p locus (often detectable by conventional karyotype and/or fluorescence in situ hybridization), 2 mutations in trans, or copy-neutral loss of heterozygosity (LOH).7 Unfortunately, it is often difficult to determine LOH with certainty without performing complex genetic analyses such as array comparative genomic hybridization or single-nucleotide polymorphism analysis. The authors did find that higher TP53 VAF (>40%) was also associated with shorter survival, although this has not been found in other studies of TP53-mutated AML.3,4 Remarkably, positive p53 immunohistochemistry pattern correlated with patients having true multihit TP53 mutations, and in and of itself was a strong predictor of both overall and leukemia-free survival.
In summary, Tashakori and colleagues have identified several genetic risk factors within the group of TP53-mutated AML (see figure). Their work confirms the utility of p53 immunohistochemistry in not only identifying TP53-mutated cases but also supplementing mutation data by providing a proteomic readout of mutations that are likely to be highly pathogenic (often due to copy-number loss, the assessment of which may not be available in many practice settings).
TP53 mutation can occur in several World Health Organization AML subtypes based on the disease ontogeny and morphology. However, the clinical behavior of AML bearing TP53 mutation appears to reflect its underlying genetic features rather than the AML category into which the disease falls. TP53-mutated AML cases with favorable or intermediate-risk karyotype, a single mutation with intact copy number status, low variant-allele fraction, and lacking an abnormal pattern of p53 protein expression by immunohistochemistry display a more favorable prognosis; conversely, the specific type of TP53 mutation does not appear to influence prognosis. t-AML, therapy-related AML; MRC, with myelodysplasia-related changes; NOS, not otherwise specified; RGA, recurrent genetic abnormalities. Professional illustration by Somersault 18:24.
TP53 mutation can occur in several World Health Organization AML subtypes based on the disease ontogeny and morphology. However, the clinical behavior of AML bearing TP53 mutation appears to reflect its underlying genetic features rather than the AML category into which the disease falls. TP53-mutated AML cases with favorable or intermediate-risk karyotype, a single mutation with intact copy number status, low variant-allele fraction, and lacking an abnormal pattern of p53 protein expression by immunohistochemistry display a more favorable prognosis; conversely, the specific type of TP53 mutation does not appear to influence prognosis. t-AML, therapy-related AML; MRC, with myelodysplasia-related changes; NOS, not otherwise specified; RGA, recurrent genetic abnormalities. Professional illustration by Somersault 18:24.
Clearly, better treatments need to be developed for patients with TP53-mutated AML, whose disease is generally chemoresistant to current therapies.8 The study of Takashori and colleagues advances us toward this goal by better defining the disease and by validating a widely available immunohistochemistry test to rapidly identify these patients in diverse practice settings. As promising therapies geared toward TP53-mutated AML become available, we are now better placed to “hit the ground running” in allocating patients appropriately to treatments and trials based on their true disease biology.
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal