Abstract
Acute myeloid leukemia (AML) remains a therapeutic challenge with high mortality rates despite intensive and myeloablative therapies. While immunotherapies targeting CD19 have yielded remarkable outcomes in acute lymphoblastic leukemia, identifying similar antigen therapeutic targets in AML remains a challenge due to inherent heterogeneity associated with AML and overlapping immunophenotypes with normal hematopoietic stem and myeloid cell populations. Transcriptional heterogeneity within pediatric AML has primarily been linked to underlying fusion. Therefore, we integrated large transcriptomics and proteomics datasets from AML and normal tissues to identify potential targets expressed in leukemias, but not in normal bone marrow or other normal tissue types.
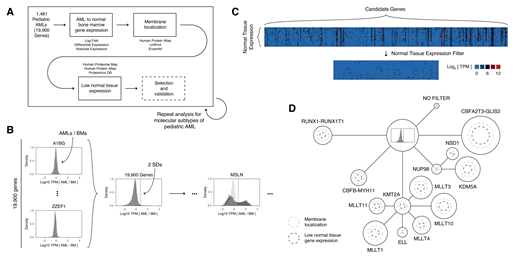
To identify candidate therapeutic targets in pediatric AML, we leveraged transcriptome sequencing data from bone marrow aspirates or peripheral blood collected from 1,481 children, adolescents, and young adults with AML at the time of diagnosis. Patients were enrolled on one of four Children's Oncology Group trials spanning the past three decades: CCG-2961, AAML03P1, AAML0531, and AAML1031. We also leveraged transcriptome sequencing from normal bone marrow (NBM) and normal CD34+ hematopoietic stem and progenitor cells (HSPCs) in order to exclude targets that are highly expressed during normal hematopoiesis. Finally, we performed additional filtering based on proteomic databases to exclude targets that lack membrane localization (Human Protein Atlas, UniProt, and Ensembl) or that are highly expressed on normal tissue types (Human Proteome Map, Human Protein Atlas, and Proteomics DB databases) (Figure 1A).
First, we computed the log expression ratio between AMLs and NBM/HSCPs for all protein coding genes. We next selected genes expressed greater than a threshold of two standard deviations above the mean in 50% or more of AMLs (Figure 1B). Additionally, we further selected genes on the basis of differential gene expression and absolute expression thresholds. This analysis was repeated for our entire pediatric AML cohort and the following AML subtypes: RUNX1-RUNX1T1, CBFB-MYH11, KMT2A-MLLT3, KMT2A-MLLT10, KMT2A-MLLT4, KMT2A-ELL, KMT2A-MLLT1, KMT2A-MLLT11, NUP98-NSD1, NUP98-KDM5A, and CBFA2T3-GLIS2. Candidate therapeutic targets were filtered based on membrane localization and normal tissue expression using the aforementioned proteomics databases (Figure 1C and 1D). Based on this algorithm, we identified a nonzero number of candidate therapeutic targets for each of our pediatric AML subtypes (Figure 1D). Intriguingly, we found no overlap between targets identified in our pediatric, adolescent, and young adult cohort and a previous similar analysis performed in AMLs diagnosed in older patients (PMID 29017060).
This study demonstrates that by combining our large transcriptomics dataset with pre-existing proteomics datasets, we are able to identify a collection of candidate therapeutic targets in pediatric AML. Importantly, zero targets were identified that were inclusive to all pediatric AMLs within our cohort, which underscores the transcriptional heterogeneity that our group and others have previously identified in pediatric AML. Future preclinical and clinical studies will need to account for this heterogeneity by prioritizing targets on the basis of underlying molecular alteration. Our study comprises a platform and dataset of candidate targets for further functional validation and/or immunotherapy targeting studies in pediatric AML.
Shaw: T-Cell and/or Gene Therapy for Cancer: Patents & Royalties.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal