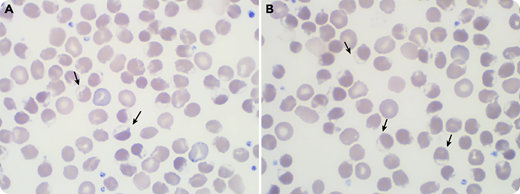
A 71-year-old white man was admitted for jaundice without fever or abdominal pain. He had received his last dose of durvalumab 2 months earlier for non–small cell lung cancer, and a first dose of anti–SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) vaccine a week earlier. The blood cell count revealed moderate anemia (120 g/L) with poikilocytosis and many bite cells (panels A-B; black arrows; original magnification ×100) on the peripheral blood smear. Within 48 hours, hemoglobin (Hb) had dropped to 48 g/L with a high reticulocyte count (250 × 109/L) and signs of hemolysis (hyperbilirubinemia: 208 µmol/L; lactate dehydrogenase: 983 U/L; haptoglobin: <0.01 g/L). Direct agglutination test (DAT) was negative. He was admitted in the intensive care unit for aspiration pneumonia, acute renal failure, and altered mental status. After a massive red blood cell infusion, the evolution was favorable. He was diagnosed with glucose-6-phosphate dehydrogenase (G6PD) deficiency with a very low G6PD rate: 0.8 UI/g Hb (reference: 11-17 UI/g).
The vaccine was first incriminated, but careful examination revealed fava bean ingestion the day before the onset of the symptoms, typically causing Hb oxidation and triggering hemolysis in the case of G6PD deficiency. He had never experienced similar symptoms. There was likely no relation between the COVID-19 vaccine or durvalumab and G6PD deficiency. This case emphasizes the cornerstone role of cytology in G6PD-deficiency diagnosis even before the onset of anemia.
A 71-year-old white man was admitted for jaundice without fever or abdominal pain. He had received his last dose of durvalumab 2 months earlier for non–small cell lung cancer, and a first dose of anti–SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) vaccine a week earlier. The blood cell count revealed moderate anemia (120 g/L) with poikilocytosis and many bite cells (panels A-B; black arrows; original magnification ×100) on the peripheral blood smear. Within 48 hours, hemoglobin (Hb) had dropped to 48 g/L with a high reticulocyte count (250 × 109/L) and signs of hemolysis (hyperbilirubinemia: 208 µmol/L; lactate dehydrogenase: 983 U/L; haptoglobin: <0.01 g/L). Direct agglutination test (DAT) was negative. He was admitted in the intensive care unit for aspiration pneumonia, acute renal failure, and altered mental status. After a massive red blood cell infusion, the evolution was favorable. He was diagnosed with glucose-6-phosphate dehydrogenase (G6PD) deficiency with a very low G6PD rate: 0.8 UI/g Hb (reference: 11-17 UI/g).
The vaccine was first incriminated, but careful examination revealed fava bean ingestion the day before the onset of the symptoms, typically causing Hb oxidation and triggering hemolysis in the case of G6PD deficiency. He had never experienced similar symptoms. There was likely no relation between the COVID-19 vaccine or durvalumab and G6PD deficiency. This case emphasizes the cornerstone role of cytology in G6PD-deficiency diagnosis even before the onset of anemia.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

Comments
Letter to the Editor
We read with interest the case of “Post-SARS-CoV-2 vaccination acute hemolysis in an older man: don’t forget to look at the blood smear”, presented by Duchemann and Lazarian in the Bloodwork section of the November 25, 2021 issue of Blood. However, we would like to bring to your attention an inaccuracy that we observed. Their case report contains two images of a peripheral blood film with many blister cells. In the text the authors refer to these as bite cells. The International Council for Standardization in Haematology (ICSH) defines bite cells as “RBC with peripheral single or multiple arcuate defects (bites) caused by the removal of Heinz bodies by the spleen . . .” and blister cells as “red cells in which the haemoglobin appears retracted into one half of the cell to form a dense mass leaving the remainder of the cell as an empty membrane”1. Secondly, Duchemann and Lazarian attribute the acute hemolysis experienced by their 71-year-old
patient to favism. However, we find it unusual that a patient with G6PD deficiency would experience a first occurrence of favism in the seventh decade of his life. Favism occurs most commonly in children between 1 and
5 years of age; this is believed to relate to the ratio of fava beans consumed to the child’s body weight.2 Additionally, patients with severe G6PD deficiency (<10% of normal), as is the case with the patient in this study, have either chronic hemolytic anemia or intermittent hemolysis.3 As such, we find it unusual that the patient did not have any history of prior similar symptoms. It may be prudent for the authors to comment whether there may have been issues with under-recognition of hemolytic symptoms by the patient and/or
healthcare constraints in accurately diagnosing prior episodes of hemolytic anemia?
References:
1. Palmer L, Briggs C, McFadden S, et al. ICSH recommendations for the standardization of nomenclature
and grading of peripheral blood cell morphological features. Int J Lab Hematol. 2015;37(3):287-303.
doi:10.1111/ijlh.12327
2. Luzzatto L, Arese P. Favism and glucose-6-phosphate dehydrogenase deficiency. N Engl J
Med. 2018;378(1):60-71.
3. Beutler E. The Molecular Biology of Enzymes of Erythrocyte Metabolism. Philadelphia, PA: W B
Saunders; 1993.