In this issue of Blood, Whitworth et al provide much needed data on thrombosis rates and risk in pediatric patients with coronavirus disease 2019 (COVID-19).1
Thrombotic events (TEs) are a frequent complication in hospitalized adults with severeCOVID-19, the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.2 Although much has been learned about TE rates and risks in adults, relatively little is known about this problem in the pediatric population. The overall incidence of COVID-19 and thrombosis is markedly lower in children, which has added challenges to studying this condition in this age group. In addition, children and adolescents are uniquely affected by a postinfectious hyperinflammatory syndrome after SARS-CoV-2 infection, termed multisystem inflammatory syndrome in children (MIS-C).3 Patients with MIS-C are also at risk for thrombosis. Given the paucity of high-quality evidence in this age group, pediatric providers have relied heavily on data extrapolated from adult studies and expert opinion for pediatric-specific guidance to manage thrombotic risk.4 The results of the study in this issue provide important information to help fill the knowledge gap in this population.
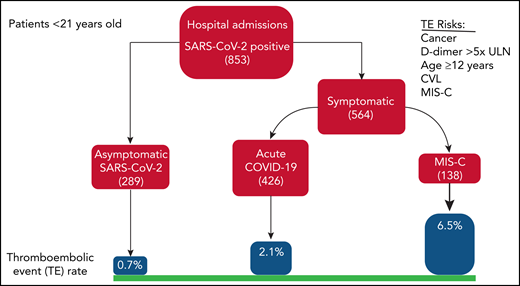
Whitworth et al describe the risks and rates of thrombosis in a multicenter retrospective cohort study of 814 children and adolescents hospitalized with SARS-CoV-2 infection across 7 pediatric hospitals in the United States. Patients younger than 21 years of age with evidence of SARS-CoV-2 infection (polymerase chain reaction positive or diagnosis of MIS-C) were included over a 5-month period (April 2020 to August 2020). The authors examined TE rates in 3 groups of patients: those with (1) asymptomatic SARS-CoV-2, (2) symptomatic COVID-19, and (3) MIS-C or MIS-C−like disease. They found a total of 20 TEs (19 with venous thromboembolism [VTE] and 1 with stroke). The TE rates in patients with SARS-CoV-2 without COVID-19 symptoms (0.7%) were similar to overall reported rates in hospitalized children (0.3% to 0.58%),5,6 suggesting that asymptomatic infection did not significantly increase risk in hospitalized patients. In patients with symptomatic acute COVID-19, the TE rate was 2.1%, and the overall TE rate in all symptomatic patients (patients with acute COVID-19 and MIS-C) was 3.2%. The risk for TE was higher in those with more severe disease needing ventilatory support and intensive care unit admission. These findings are consistent with other reports: a multi-institutional cohort study from the Tri-State Pediatric COVID-19 Research Consortium found an overall TE rate (in COVID-19 and MIS-C) of 4.3% and a rate of 7.7% in patients with respiratory symptoms.7 In this current study, the group of patients diagnosed with the postinfectious inflammatory syndrome, MIS-C, had the highest TE rate at 6.5%, which is similar to the 8% rate reported from a national surveillance study in patients with MIS-C.8 The development of TE with COVID-19 infection was associated with poor outcomes in children as has been described in adults. In pediatric patients, the mortality rate was 28% with TE compared with 1% without TE, and most who died had significant comorbidities. In adults with COVID-19, the pooled estimate of mortality with TE is 23% compared with 13% without TE (see figure).2
Several observations parallel what has been seen in adults. Whitworth et al reported that over two-thirds of patients developed TE (71%) despite anticoagulant prophylaxis, in line with the high rates of VTE reported in adults treated with anticoagulant prophylaxis. In adults, D-dimer elevation has been shown to be correlated with disease severity and TE, however, this has not been previously demonstrated as a risk in children. A D-dimer increase of 5 times above the upper limit of normal was found to be significantly associated with TE in a multivariable analysis. These findings may reflect a common pathology that spans all age ranges. In contrast, several comorbidities associated with severe disease in adults were not associated with TE in children, including obesity, cardiac disease, and sickle cell disease, although small sample sizes for these conditions limit conclusions. One additional finding to note was the increased prevalence of TE found in African American race and Hispanic ethnicity; this is also reported in adults with COVID-19, reminding us that children are not immune to the racial disparities seen with this disease.
A challenge for managing thrombotic risk in the pediatric population is deciding who is most likely to benefit from anticoagulation prophylaxis and who is likely to be harmed. With TE rates so much lower in children than adults, a blanket approach using thromboprophylaxis for all patients with COVID-19 in this age group may unnecessarily expose low-risk patients to bleeding. This study identified a number of risk factors for TE that have been found in other pediatric studies, including older age (≥12 years), malignancy, and central lines.6,9 These factors, in combination with disease severity, ventilatory support, and D-dimer elevation, could be used for risk stratification. More high-quality data are needed to develop and validate a robust risk-assessment model to guide prophylaxis approaches.
What are the remaining questions? Given the high incidence of thrombosis despite thromboprophylaxis in this study, as seen in adults, the optimal intensity and type of anticoagulation need to be determined. Similarly, the appropriate duration of anticoagulation and the role of postdischarge prophylaxis are, thus far, unstudied in children. The relatively low incidence of TEs requires large data sets, patient registries, and multi-institutional collaborations, as used in this project, to obtain high-quality evidence to optimally manage this risk in pediatric patients; however, additional studies are needed. This current study provides valuable information that can be used to develop thromboprophylaxis approaches in children with COVID-19.
TEs in pediatric patients with SARS-CoV-2 infection. Hospitalized patients <21 years of age were stratified into (1) asymptomatic SARS-CoV-2, (2) symptomatic COVID-19, and (3) MIS-C or MIS-C–like disease. Thrombotic event rates are thrombotic risks are listed. CVL, central venous catheter; ULN, upper limit of normal.
TEs in pediatric patients with SARS-CoV-2 infection. Hospitalized patients <21 years of age were stratified into (1) asymptomatic SARS-CoV-2, (2) symptomatic COVID-19, and (3) MIS-C or MIS-C–like disease. Thrombotic event rates are thrombotic risks are listed. CVL, central venous catheter; ULN, upper limit of normal.
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal