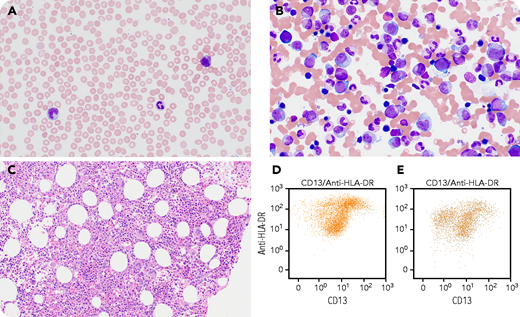
A 67-year-old man presented with increased fatigue, spontaneous bruising on his thighs, new inflammation of his wrist, relapsing polychondritis, and macrocytic anemia. The peripheral blood shows slight anisocytosis and left-shifted granulocytes with 10% myelocytes (panel A, peripheral blood smear, Wright-Giemsa stain, objective magnification 60×, total magnification ×600). Besides the occasional cytoplasmic vacuoles in myeloid cells identified in the bone marrow aspirate, bone marrow biopsy and aspirate show moderate hypercellularity with essentially normal trilineage hematopoiesis (panel B, bone marrow aspirate, Wright-Giemsa stain, objective magnification 60×, total magnification ×600; panel C, hematoxylin and eosin stain, objective magnification 20×, total magnification ×200). Flow cytometric immunophenotyping showed an atypical pattern of myeloid maturation (panel D, HLA-DR/CD13; panel E, normal pattern). Molecular analysis for UBA1 gene revealed a mutation (UBA1 c.121A>G, p.Met41Val), confirming the diagnosis of vacuoles, E1 enzyme, X-linked, autoinflammatory, and somatic (VEXAS) syndrome.
VEXAS syndrome is mostly the result of a missense somatic mutation affecting methionine-41 (p.Met41) of the X-linked gene UBA1, which encodes E1 ubiquitin-activating enzyme. Patients with VEXAS syndrome typically show cytopenia, dysplasia, and cytoplasmic vacuoles in myeloid and erythroid cells in addition to the inflammatory manifestations including fever, relapsing chondritis, and vasculitis. The subtle morphologic features of this case suggest a low threshold of performing UBA1 mutation testing in the presence of cytopenia and inflammatory syndrome.
A 67-year-old man presented with increased fatigue, spontaneous bruising on his thighs, new inflammation of his wrist, relapsing polychondritis, and macrocytic anemia. The peripheral blood shows slight anisocytosis and left-shifted granulocytes with 10% myelocytes (panel A, peripheral blood smear, Wright-Giemsa stain, objective magnification 60×, total magnification ×600). Besides the occasional cytoplasmic vacuoles in myeloid cells identified in the bone marrow aspirate, bone marrow biopsy and aspirate show moderate hypercellularity with essentially normal trilineage hematopoiesis (panel B, bone marrow aspirate, Wright-Giemsa stain, objective magnification 60×, total magnification ×600; panel C, hematoxylin and eosin stain, objective magnification 20×, total magnification ×200). Flow cytometric immunophenotyping showed an atypical pattern of myeloid maturation (panel D, HLA-DR/CD13; panel E, normal pattern). Molecular analysis for UBA1 gene revealed a mutation (UBA1 c.121A>G, p.Met41Val), confirming the diagnosis of vacuoles, E1 enzyme, X-linked, autoinflammatory, and somatic (VEXAS) syndrome.
VEXAS syndrome is mostly the result of a missense somatic mutation affecting methionine-41 (p.Met41) of the X-linked gene UBA1, which encodes E1 ubiquitin-activating enzyme. Patients with VEXAS syndrome typically show cytopenia, dysplasia, and cytoplasmic vacuoles in myeloid and erythroid cells in addition to the inflammatory manifestations including fever, relapsing chondritis, and vasculitis. The subtle morphologic features of this case suggest a low threshold of performing UBA1 mutation testing in the presence of cytopenia and inflammatory syndrome.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal