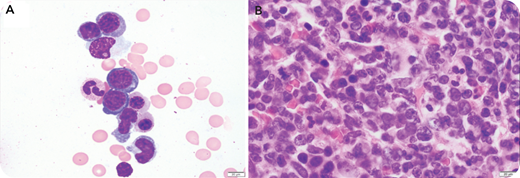
A 65-year-old man was diagnosed with immunoglobulin G lambda (IgG lambda) plasma cell myeloma in July 2019 with 70% involvement of bone marrow. He was positive for t(11;14) via fluorescent in situ hybridization (FISH) cytogenetics testing, and he had immunoglobulin heavy chain (IgH) gene rearrangement and 4 copies of Tp53. He received induction therapy with bortezomib, lenalidomide, dexamethasone and maintenance therapy with dexamethasone, and he also had an autologous stem cell transplantation in December 2019. He underwent bone marrow biopsy during a 3-month posttransplant follow-up. The peripheral blood showed mild normocytic normochromic anemia, thrombocytopenia, and rare scattered plasma cells. The bone marrow aspirate showed scattered abnormal plasma cells, several of which had irregular or convoluted nuclei and delicate blue cytoplasm with vacuoles (panel A, 400× objective). The core biopsy showed sheets of abnormal plasma cells, many of which had convoluted or horseshoe-shaped nuclei (panel B, 1000× objective). These cells stained positive for CD138 and CD56 and were negative for CD20 and CD30. The FISH cytogenetics panel was positive for t(11;14) with extra copies of the IgH gene.
This unique morphology of plasma cells, which included anisocytosis, irregular nuclear shape, and cytoplasmic vacuoles, can be seen in progressive disease and may be related to poor prognosis. This unique morphology can be mistaken for a myeloid neoplasm in the aspirate or a non-Hodgkin lymphoma in a biopsy and warrants ancillary testing to confirm the diagnosis.
A 65-year-old man was diagnosed with immunoglobulin G lambda (IgG lambda) plasma cell myeloma in July 2019 with 70% involvement of bone marrow. He was positive for t(11;14) via fluorescent in situ hybridization (FISH) cytogenetics testing, and he had immunoglobulin heavy chain (IgH) gene rearrangement and 4 copies of Tp53. He received induction therapy with bortezomib, lenalidomide, dexamethasone and maintenance therapy with dexamethasone, and he also had an autologous stem cell transplantation in December 2019. He underwent bone marrow biopsy during a 3-month posttransplant follow-up. The peripheral blood showed mild normocytic normochromic anemia, thrombocytopenia, and rare scattered plasma cells. The bone marrow aspirate showed scattered abnormal plasma cells, several of which had irregular or convoluted nuclei and delicate blue cytoplasm with vacuoles (panel A, 400× objective). The core biopsy showed sheets of abnormal plasma cells, many of which had convoluted or horseshoe-shaped nuclei (panel B, 1000× objective). These cells stained positive for CD138 and CD56 and were negative for CD20 and CD30. The FISH cytogenetics panel was positive for t(11;14) with extra copies of the IgH gene.
This unique morphology of plasma cells, which included anisocytosis, irregular nuclear shape, and cytoplasmic vacuoles, can be seen in progressive disease and may be related to poor prognosis. This unique morphology can be mistaken for a myeloid neoplasm in the aspirate or a non-Hodgkin lymphoma in a biopsy and warrants ancillary testing to confirm the diagnosis.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal