High-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements (also called double-hit [or triple-hit] diffuse large B-cell lymphoma [DLBCL]) is a distinct biological entity associated with kinetically aggressive disease, high rates of central nervous system involvement, and inferior clinical outcomes. In this issue of Blood, Collinge et al build on their previous work and further dissect the definition of this entity through the lens of the diagnostic tools currently available to pathologists.1
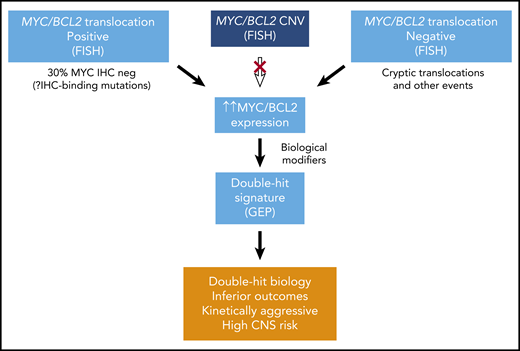
Identifying double-hit lymphoma biology using diagnostic tools. CNS, central nervous system; CNV, copy number variation; GEP, gene expression profiling.
Identifying double-hit lymphoma biology using diagnostic tools. CNS, central nervous system; CNV, copy number variation; GEP, gene expression profiling.
In 2020, cell morphology as assessed by the light microscope, for better or for worse, retains its place in the diagnostic armory used to stratify lymphoma into biologically and prognostically relevant groups. After initial subcategorization by microscopic features, there is now an ever-expanding array of downstream diagnostic tools and technologies that are increasingly relied upon to provide further biological insight in order to inform patient management (see figure). High-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements is a recently recognized entity by the World Health Organization (WHO) whose definition is reliant on these technologies and hostage to their limitations.2 Although this entity is currently defined by the presence of structural variants involving MYC and BCL2+/−BCL6 (typically detected by fluorescence in situ hybridization [FISH]), it is clear that the “true” double-hit lymphoma biological entity extends far beyond those with detectable abnormalities by conventional FISH testing. A major step toward biological bedrock was the development of a specific gene expression signature that could identify double-hit lymphoma biology, which revealed that ∼50% of patients with the clinicobiological features of double-hit lymphoma was unrecognized by conventional FISH testing.3 Although this may be related in part to the technical performance and discordance of commonly used FISH probes,4 subsequent whole-genome sequencing studies have shown that ∼30% of these patients harbor translocations of MYC/BCL2/BCL6 loci that are cryptic to FISH.5 However, despite the improved pickup rate when using high-resolution massively parallel sequencing technologies, there is still a significant proportion of patients that belong to the true biological double-hit lymphoma subgroup as defined by gene expression profiling, that do not harbor classical translocations of these loci.
This study by Collinge et al investigates other potential pathways to double-hit lymphoma biology. Using a gene expression signature developed on a cohort of high-grade B-cell lymphoma with BCL2 rearrangements, double or triple hit, to define true biological double-hit lymphoma, the authors first show that copy number gains of MYC (present in ∼20% to 25% of patients) do not routinely lead to MYC overexpression and are not equivalent to MYC translocations in that they do not lead to double-hit lymphoma biology. Likewise, copy number gains of BCL2 (despite their association with overexpression) were also shown to be nonequivalent to BCL2 translocations with regard to double-hit lymphoma biology. Further study is required to determine whether the biological basis of this observation relates to a specific requirement of the regulatory region of the partner chromosome (immunoglobulin locus or otherwise), and furthermore, how different MYC/BCL2 translocation partners may also affect the biological outcome. In addition, the impact of BCL6 genomic abnormalities as well as any effect of histological features, such as blastoid morphology, also remains to be elucidated. However, regardless of the underlying mechanism, these findings indicate that we have more or less reached the limit of FISH to identify cases of true biological double-hit lymphoma, which falls significantly short of identifying the entire population of interest.
Immunohistochemistry (IHC) staining for MYC has previously been investigated as a means of triaging those patients in whom FISH testing is warranted to detect MYC translocations. Although this approach was used by diagnostic laboratories initially, it has since become clear that a significant proportion of patients harboring MYC translocations (30% in the current study) are “negative” for MYC staining by IHC. One mechanism of false-negative staining (ie, negative MYC IHC in the presence of increased MYC expression) that has been reported in this work is the presence of a relatively rare (2% to 3%) germline polymorphism, NM_002467.4:c.77A>G; p.(Asn26Ser) (referred to in this work as MYC-N11S), that disrupts the binding epitope of a commonly used IHC clone (Y69). It is also highly likely that other mutations (both germline and acquired through aberrant somatic hypermutation of MYC) will result in false-negative MYC IHC staining in a proportion of cases and further reinforces that IHC cannot be routinely relied upon to triage cases prior to FISH testing when pursuing a diagnosis of double-hit lymphoma.
The limitations of FISH and IHC in this context for identifying double-hit biology raise the question of whether gene expression profiling should be routinely used clinically to identify this important subtype. There is little doubt that gene expression profiling is a powerful method for accurate identification of double-hit lymphoma (as well as Burkitt lymphoma, primary mediastinal B-cell lymphoma, DLBCL cell of origin, T-cell lymphoma subtyping, and others); however, up until now this technique has not been widely implemented into routine diagnostic hematopathology practice. Although the reasons for this may be related to technical (instrumentation, bioinformatics support, availability of appropriate tissue) or financial considerations, it may equally be related to the lack of an evidence-based clinical intervention to improve outcomes based on the results of these specific signatures. Regardless, there is little doubt that the prerequisite for improving outcomes in patients with DLBCL (and hematological malignancy more broadly) is to accurately establish the patient’s diagnosis with appropriate respect to conventional WHO criteria as well as the molecular and biological phenotype. In 2020, the light microscope, one of the great survivors in the pantheon of scientific instruments, retains its relevance; however, there is clearly further work to do to optimize and effectively implement downstream technologies to fully capture double-hit lymphoma.
Conflict-of-interest disclosure: The authors declare no competing financial interests.