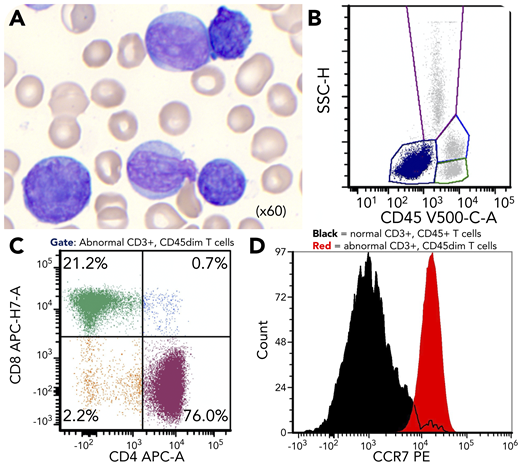
A 59-year-old man with cirrhosis admitted for methicillin-susceptible Staphylococcus aureus bacteremia was found to have hyperleukocytosis (white blood cell count 225 109/L). Peripheral blood showed polymorphic lymphocytes: large with irregular nuclear contours, medium with prominent nucleoli, and small with cytoplasmic projections (panel A; Wright-Giemsa, original magnification ×60). Flow cytometry showed an abnormal CD45 dim/negative population (panel B), which was a polytypic mixture of 4 mature CD3+ T-cell populations with a normal CD4:CD8 ratio (∼3:1) (panel C). The predominant population (76% of abnormal T cells) showed low side scatter, expressed CD4 and all pan-T antigens, and was negative for immature markers (CD34/TdT/CD1a). Separate abnormal CD8+, CD4/CD8 double-negative, and CD4/CD8 double-positive T-cell populations comprising 20%, 2%, and 0.7% of abnormal T cells, respectively, expressed a similar immunophenotype but showed variation in forward and side scatter. Human T-cell lymphotropic virus type 1/2 serology was negative. ATM T2947N and JAK3 A573V mutations were identified at variant allele frequencies (VAFs) of 94% and 38%, respectively, and fluorescence in situ hybridization showed TCL1A gene rearrangement in 78% of nuclei.
This is a case of “polytypic” T-cell prolymphocytic leukemia (T-PLL) with 4 distinct subpopulations differing based on morphology, forward/side scatter, and CD4/CD8 coexpression. Although clonal in nature based on TCL1A gene rearrangement, the difference in VAFs between ATM and JAK3 mutations suggests that neoplastic T-PLL cells can also show genetic heterogeneity. Last, T-PLL demonstrates high expression of CCR7 (panel D), a possible future therapeutic target.
A 59-year-old man with cirrhosis admitted for methicillin-susceptible Staphylococcus aureus bacteremia was found to have hyperleukocytosis (white blood cell count 225 109/L). Peripheral blood showed polymorphic lymphocytes: large with irregular nuclear contours, medium with prominent nucleoli, and small with cytoplasmic projections (panel A; Wright-Giemsa, original magnification ×60). Flow cytometry showed an abnormal CD45 dim/negative population (panel B), which was a polytypic mixture of 4 mature CD3+ T-cell populations with a normal CD4:CD8 ratio (∼3:1) (panel C). The predominant population (76% of abnormal T cells) showed low side scatter, expressed CD4 and all pan-T antigens, and was negative for immature markers (CD34/TdT/CD1a). Separate abnormal CD8+, CD4/CD8 double-negative, and CD4/CD8 double-positive T-cell populations comprising 20%, 2%, and 0.7% of abnormal T cells, respectively, expressed a similar immunophenotype but showed variation in forward and side scatter. Human T-cell lymphotropic virus type 1/2 serology was negative. ATM T2947N and JAK3 A573V mutations were identified at variant allele frequencies (VAFs) of 94% and 38%, respectively, and fluorescence in situ hybridization showed TCL1A gene rearrangement in 78% of nuclei.
This is a case of “polytypic” T-cell prolymphocytic leukemia (T-PLL) with 4 distinct subpopulations differing based on morphology, forward/side scatter, and CD4/CD8 coexpression. Although clonal in nature based on TCL1A gene rearrangement, the difference in VAFs between ATM and JAK3 mutations suggests that neoplastic T-PLL cells can also show genetic heterogeneity. Last, T-PLL demonstrates high expression of CCR7 (panel D), a possible future therapeutic target.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal