Background:
The rapid global spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), remains the international public health concern of the decade. Early clinical data suggest that patients (pts) with hematologic malignancies are vulnerable to severe forms of SARS-CoV-2 and have higher mortality rates than the general population.
Greater understanding of risk factors and outcomes associated with SARS-CoV-2 in pts with hematologic malignancies is crucial in order to develop individualized risk-benefit analyses to guide care. Herein, we report a cohort study from a Comprehensive Cancer Center evaluating outcomes in pts with hematologic malignancies who developed SARS-CoV-2.
Methods:
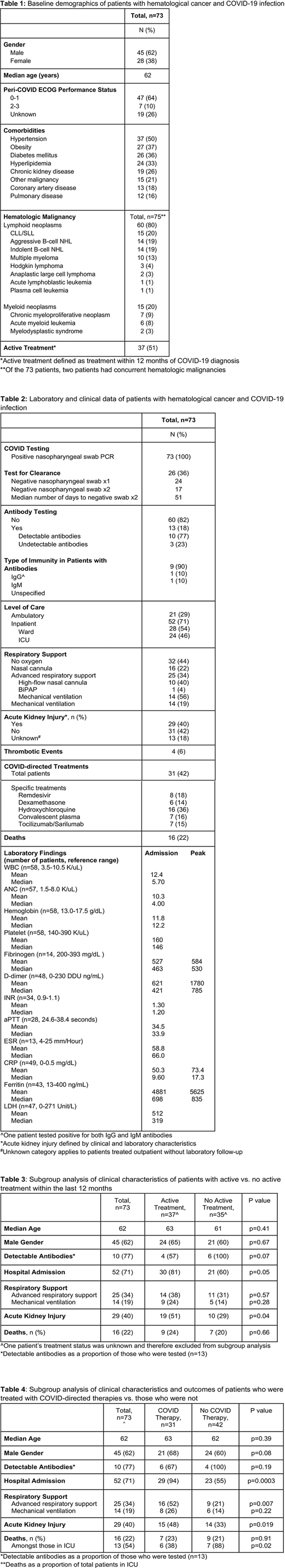
Adult pts at Northwestern Memorial Hospital with a current/prior hematologic malignancy and laboratory-confirmed SARS-CoV-2 infection confirmed by quantitative RT-PCR from nasopharyngeal swabs between March-July, 2020 were identified using electronic health records. Data were collected and analyzed based on epidemiologic, laboratory, and clinical characteristics.
Severity of illness was defined by level of care (ambulatory, inpatient), need for advanced respiratory support (high flow nasal cannula, BiPAP, mechanical ventilation), incidence of thrombotic events, incidence of acute kidney injury (AKI), and/or death.
Statistical analyses of risk factors, severity, and outcomes were performed. Subgroup analyses based on antineoplastic treatment status and receipt of SARS-CoV-2 -directed therapy were made. Active cancer treatment was defined as antineoplastic therapy within 12 months of SARS-CoV-2 diagnosis.
Results:
Demographic (Table 1) and clinical (Table 2) data were recorded from 73 SARS-CoV-2 infected pts. Sixty (80%) pts had lymphoid and 15 (20%) had myeloid neoplasms, 2 with concurrent lymphoid and myeloid neoplasms. Thirty-seven (51%) pts were undergoing active treatment for their malignancy.
Twenty-one pts (29%) were managed in the ambulatory setting while 52 (71%) required hospital admission. Twenty-five (34%) pts required advanced respiratory support including 14 (19%) who required mechanical ventilation. Four pts (6%) had thrombotic events and 31 (42%) received SARS-CoV-2-directed therapies. Sixteen pts (22%) died during the study period.
Pts on active cancer treatment had higher rates of hospital admission (81% v 60%; p=0.05) and AKI (51% v 29%; p=0.04) but similar rates of death compared with pts not on active treatment (24% v 20%; p=0.66) (Table 3). Comparing pts who received SARS-CoV-2 -directed therapy versus no therapy: pts on therapy had longer median lengths of stay (11 v 7 days; p=0.04) and higher rates of hospital admission (94% v 55%; p=0.0003) but similar rates of death (23% v 21%; p=0.91); pts in the ICU on SARS-COV-2 -directed therapy had lower rates of death (38% v 88% p=0.02) than pts who did not receive such therapy (Table 4).
Twenty-six pts (36%) were tested for viral clearance, defined as two serial negative swabs ≥24 hours apart. Of these, 17 (65%) achieved clearance with a median time of 51 days (range 15-119 days).
Thirteen pts (18%) had antibody (Ab) testing. Ten (77%) had detectable Abs: 8 were positive for IgG, 1 for IgG and IgM, and 1 had unspecified positivity. Notably, all 3 pts with undetectable Abs were on active cancer treatment.
Conclusion:
We demonstrate that pts with hematologic malignancies are exceptionally vulnerable to severe forms of SARS-CoV-2 with high mortality rates. The incidence of thrombotic events was low, an unexpected finding in the setting of a hyperinflammatory syndrome.
Prolonged time to viral clearance was observed, a finding which may cause potential delays in the resumption of cancer-directed therapies. Notably, the majority of pts who received antibody testing had detectable antibodies suggesting that pts with hematologic malignancies may be able to mount an immune response to early vaccination.
Accordingly, close monitoring, aggressive therapy, and early vaccination, when available, may be warranted for this population.
Larger studies are needed to confirm our findings and help guide management of pts with hematologic malignancies during the SARS-CoV-2 pandemic.
Altman:Bristol-Myers Squibb: Consultancy; Janssen: Consultancy; Immune Pharmaceuticals: Consultancy; Syros: Consultancy; Genentech: Research Funding; Novartis: Consultancy; Amphivena: Research Funding; Amgen: Research Funding; Aprea: Research Funding; ImmunoGen: Research Funding; Celgene: Research Funding; Boehringer Ingelheim: Research Funding; Fujifilm: Research Funding; Kartos: Research Funding; AbbVie: Other: advisory board, Research Funding; Kura Oncology: Other: Scientific Advisory Board - no payment accepted, Research Funding; BioSight: Other: No payment but was reimbursed for travel , Research Funding; Daiichi Sankyo: Other: Advisory Board - no payment but was reimbursed for travel; Agios: Other: advisory board, Research Funding; Glycomimetics: Other: Data safety and monitoring committee; Astellas: Other: Advisory Board, Speaker (no payment), Steering Committee (no payment), Research Funding; Theradex: Other: Advisory Board; ASH: Consultancy; Cancer Expert Now: Consultancy; France Foundation: Consultancy; PeerView: Consultancy; PrIME Oncology: Consultancy. Winter:Delta Fly Pharma: Consultancy; Amgen: Consultancy; Epizyme: Other: DSMB; CVS/Caremark: Consultancy; Ariad/Takeda: Consultancy; Norvartis: Consultancy, Other: DSMB; Merck: Membership on an entity's Board of Directors or advisory committees, Other: advisory board; Karyopharm: Membership on an entity's Board of Directors or advisory committees, Other: advisory board. Gordon:Zylem Biosciences: Patents & Royalties: Patents, No Royalties. Pro:Verastem Oncology: Research Funding. Ma:TG Therapeutics: Research Funding; Juno: Research Funding; Novartis: Research Funding; Kite: Consultancy, Honoraria; Pharmacyclics, LLC, an AbbVie Company: Consultancy, Honoraria, Research Funding, Speakers Bureau; AbbVie: Consultancy, Honoraria, Research Funding; AstraZeneca: Consultancy, Honoraria, Research Funding, Speakers Bureau; BeiGene: Honoraria, Research Funding, Speakers Bureau; Bioverativ: Consultancy, Honoraria; Genentech: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; Janssen: Consultancy, Honoraria, Research Funding, Speakers Bureau. Karmali:BMS/Celgene/Juno: Honoraria, Other, Research Funding, Speakers Bureau; Takeda: Research Funding; Karyopharm: Honoraria; Gilead/Kite: Honoraria, Other, Research Funding, Speakers Bureau; AstraZeneca: Speakers Bureau; BeiGene: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal