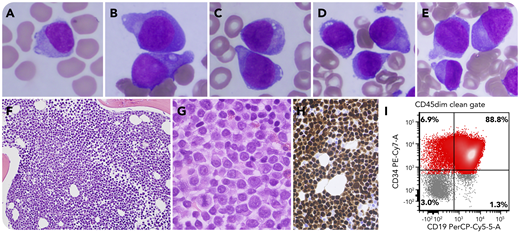
A 65-year-old woman with a history of multiple myeloma, diploid karyotype, in remission 5 years after double autologous stem cell transplant, was on maintenance therapy with elotuzumab and lenalidomide. Upon follow-up, she was found to have pancytopenia with 24% circulating “plasmacytoid” cells (panel A: Wright-Giemsa stain, original magnification ×1000). No paraprotein was detected. Bone marrow evaluation showed a hypercellular marrow replaced by medium-sized plasmacytoid cells, 85% of cellularity, characterized by immature chromatin, prominent nucleoli, and few cytoplasmic vacuoles (panels B-E: Wright-Giemsa stain, original magnification ×1000; panels F-G: hematoxylin and eosin stain, original magnification ×200 and ×1000, respectively). The neoplastic cells expressed PAX-5 and TdT (panel H: original magnification ×400) by immunohistochemistry; they were also CD45dim and expressed CD19, CD22, and CD34 by flow cytometry (panel I). The patient was diagnosed with B acute lymphoblastic leukemia. No aberrant plasma cell population was detected. Conventional karyotyping showed trisomy 8. Mutation profiling revealed 2 TP53 missense mutations, A347T and P177L. Fluorescence in situ hybridization was negative for deletion of the 17p13.1/TP53 locus.
This case emphasizes the importance of considering the emergence of B acute lymphoblastic leukemia in patients with history of multiple myeloma, especially in cases with plasmacytoid morphology that might mimic plasma cell leukemia. Whether multiple myeloma treatment could result in therapy-related B acute lymphoblastic leukemia remains to be elucidated.
A 65-year-old woman with a history of multiple myeloma, diploid karyotype, in remission 5 years after double autologous stem cell transplant, was on maintenance therapy with elotuzumab and lenalidomide. Upon follow-up, she was found to have pancytopenia with 24% circulating “plasmacytoid” cells (panel A: Wright-Giemsa stain, original magnification ×1000). No paraprotein was detected. Bone marrow evaluation showed a hypercellular marrow replaced by medium-sized plasmacytoid cells, 85% of cellularity, characterized by immature chromatin, prominent nucleoli, and few cytoplasmic vacuoles (panels B-E: Wright-Giemsa stain, original magnification ×1000; panels F-G: hematoxylin and eosin stain, original magnification ×200 and ×1000, respectively). The neoplastic cells expressed PAX-5 and TdT (panel H: original magnification ×400) by immunohistochemistry; they were also CD45dim and expressed CD19, CD22, and CD34 by flow cytometry (panel I). The patient was diagnosed with B acute lymphoblastic leukemia. No aberrant plasma cell population was detected. Conventional karyotyping showed trisomy 8. Mutation profiling revealed 2 TP53 missense mutations, A347T and P177L. Fluorescence in situ hybridization was negative for deletion of the 17p13.1/TP53 locus.
This case emphasizes the importance of considering the emergence of B acute lymphoblastic leukemia in patients with history of multiple myeloma, especially in cases with plasmacytoid morphology that might mimic plasma cell leukemia. Whether multiple myeloma treatment could result in therapy-related B acute lymphoblastic leukemia remains to be elucidated.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

Comments
increased rate of B-ALL in CLL patients treated with Lenalidomide