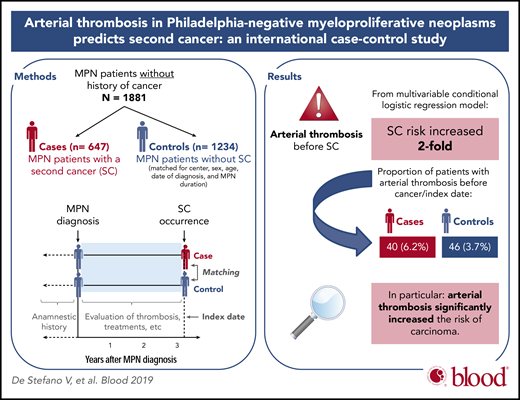
In this issue of Blood, De Stefano and colleagues report that the occurrence of an arterial thrombotic event during follow-up after the diagnosis of a Philadelphia chromosome–negative myeloproliferative neoplasm (MPN) is independently associated with a significantly increased risk of second primary nonhematologic, nondermatologic cancer.1
See the visual abstract in the online version of the article by De Stefano et al that begins on page 381.
See the visual abstract in the online version of the article by De Stefano et al that begins on page 381.
The natural history of MPNs, including essential thrombocythemia (ET), polycythemia vera (PV), and primary myelofibrosis (PMF), involves cardiovascular thrombotic events, hematologic transformation to acute myeloid leukemia, and cumulative incidence of second, nonhematologic cancer up to 12.7% at 10 years.2 Rates of cardiovascular events are significantly higher in patients with MPN compared with matched control population across all age groups, with arterial events being more frequent than venous thrombosis.3 At diagnosis of MPN, in a review of 13 436 patients, the prevalence of arterial and venous thrombosis was 16.2% and 6.2%, respectively.4 During follow-up of patients with ET and PV, vascular complications were associated with significantly inferior survival in a recent study of 1685 patients, although causes of death remain to be reported.5 Cardiovascular events have long been recognized as significant contributors to morbidity and potential mortality in patients with MPN; however, the association between occurrence of arterial or venous thrombotic complications and risk of subsequent development of second primary cancer (SC) had not been investigated to date.
Using a nested case-control study design,6 De Stefano and colleagues recruited cases of patients with MPN from 30 European Leukemia Net (ELN) centers with a diagnosis of SC and carefully matched up to 3 control patients without SC for each case (see figure). Although thrombosis frequency preceding MPN diagnosis was similar in ∼20% in each cohort, thrombotic event frequency was significantly higher after MPN diagnosis and before SC diagnosis in cases compared with controls. This increased frequency was accounted for by a significantly higher proportion of arterial (and not venous) thrombosis observed in cases compared with controls (6.2% vs 3.7%, P = .015). Furthermore, among patients with venous thrombosis, although there were relatively few cases, splanchnic vein thrombosis during follow-up was significantly more common in cases with nonhematologic, nondermatologic carcinomas compared with controls. Whereas the cumulative incidence of arterial thrombosis over time was significantly higher in cases with SC compared with controls, there was no significant difference in cumulative incidence of venous thrombosis between groups. Interestingly, the incidence of subsequent SC following venous thrombosis in patients with MPN was similar to the general population with unprovoked venous thromboembolism. Also noteworthy is that patients with recurrent thrombosis during follow-up had a higher risk of SC compared with patients who experienced no thrombosis.
Another interesting and important finding is that low-dose aspirin thromboprophylaxis during follow-up was associated with a significant protective effect against nonhematologic, nondermatologic cancer (odds ratio, 0.64; 95% confidence interval [CI], 0.47-0.87). The majority of patients (76% of cases and 80% of controls) received low-dose aspirin, likely per ELN guidelines, as secondary prophylaxis of thrombosis or as primary prophylaxis in PV.7 The authors investigated this finding further in an effort to reconcile the observed protective effect of low-dose aspirin in patients with MPN with the previously unexpected finding of increased cancer-related mortality in healthy, elderly individuals randomized to low-dose daily aspirin.8 Further analyses revealed that aspirin (dose, 100 mg; median exposure time, 4.5 years) was associated specifically with risk reduction of female genital cancers, including ovarian, endometrial, and breast cancer (odds ratio, 0.47; 95% CI, 0.25-0.89), consistent with a favorable effect of low-dose aspirin reported in other studies.9 Of note, there was no effect of aspirin in this MPN cohort on frequency of other cancer types, including colorectal carcinoma, as well as dermatologic and hematologic cancers. These interesting findings provide rationale for further studies designed to investigate low-dose aspirin as a modulator of SC incidence in patients with MPN, beyond its role as a primary thromboprophylaxis agent, which requires further definition, particularly in patients with ET and PMF.
Regarding cytoreductive therapy during follow-up and potential association with thrombosis and SC development, the majority of patients with MPN, ∼70% in both cohorts, received hydroxyurea. There were no differences in rates of arterial or venous thrombosis during treatment with hydroxyurea between cases with SC and controls. However, in the absence of treatment with hydroxyurea, the proportion of arterial thrombosis was significantly higher in cases with SC. As reported recently in this cohort of patients,6 hydroxyurea was associated with increased nonmelanoma skin cancer, but not with nonhematologic solid tumors or hematologic SC, the latter a matter of intense discussion within the MPN community for decades. It is important to note that the median duration of hydroxyurea exposure was relatively short (3 years; range, 1.2 to 6.1) precluding a firm conclusion based on available data at this time.6 A more recent analysis of this MPN cohort reported that SCs constitute a major cause of death and that exposure to specific cytoreductive agents such as hydroxyurea or ruxolitinib since MPN diagnosis may be associated with significantly inferior outcomes after SC diagnosis, clearly another area that requires future research and confirmation.10
The novel findings of this study by De Stefano and colleagues are important, because the data (1) sheds new light on a previously unrecognized clinical and prognostic implication of arterial thrombosis, one of the most concerning and potentially devastating complications that may occur during the course of MPNs; and (2) provides an opportunity for intervention in the clinic in an effort to improve outcomes. Elucidation of the pathogenesis of SCs in patients with MPN, specifically the role of potentially oncogenic or preventive therapies, and the interplay of disease-specific and host-related factors, requires further study. De Stefano and colleagues show that arterial thrombosis or splanchnic vein thrombosis occurring during follow-up after MPN diagnosis is a harbinger of increased risk of SCs, primarily solid tumors. The 5 most frequent carcinoma types encountered included prostate, breast, colorectal, lung, and gynecologic cancers, all of which are amenable to screening and early detection strategies per established guidelines. Thus, for patients with MPN whose course is complicated by an arterial thrombotic event, heightened vigilance and careful sex- and age-appropriate clinical surveillance for early diagnosis of SC are indicated as recommended by the authors.
Conflict-of-interest disclosure: M.O.A. declares no competing financial interests.