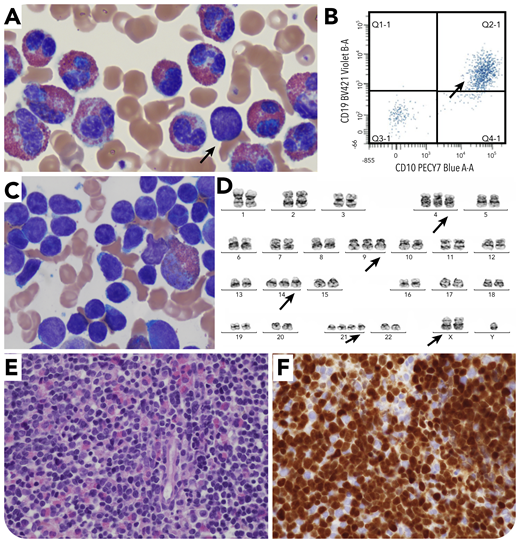
A 13-year-old boy with autism spectrum disorder presented to the Emergency Department with left flank pain and hepatosplenomegaly. Laboratory workup showed an absolute eosinophil count of 65 280 × 109/L and white blood cell count of 88 200 × 109/L in the absence of anemia or thrombocytopenia. Peripheral smear review confirmed marked eosinophilia (75%) with very few (1%) circulating lymphoblasts (panel A; Wright-Giemsa, original magnification ×100), positive by flow cytometry for CD10 (bright) and CD19 (panel B), along with CD34, TDT, CD22, cCD79a, HLA-DR, CD9, CD58, and CD123. Bone marrow examination showed 70% to 80% involvement by B-lymphoblastic leukemia/lymphoma (B-ALL), with aspirate demonstrating sheets of blasts admixed with eosinophils/eosinophilic precursors (panel C; Wright-Giemsa, original magnification ×100). The core biopsy showed 70% to 80% B-ALL lymphoblasts (panel E; hematoxylin and eosin, original magnification ×40), which are TDT positive (panel F; TDT, original magnification ×40), along with admixed eosinophils/eosinophilic precursors. The cytogenetic study showed high hyperdiploid karyotype: 52,XY,+X,+4,+9,+14,+21,+21 (panel D). The most common translocation t(5;14) (q31;q32) associated with B-ALL cases with hypereosinophilia, as well as relatively less common recurrent abnormalities such as translocation t(7;12)(q22;p13) and deletions involving 5q, 7q, were not identified.
The current study highlights the need for high suspicion of B-ALL and bone marrow examination in a hypereosinophilia case presenting with very few or no circulating lymphoblasts. The hyperdiploid karyotype is an example of cytogenetic diversity of B-ALL cases associated with hypereosinophilia.
A 13-year-old boy with autism spectrum disorder presented to the Emergency Department with left flank pain and hepatosplenomegaly. Laboratory workup showed an absolute eosinophil count of 65 280 × 109/L and white blood cell count of 88 200 × 109/L in the absence of anemia or thrombocytopenia. Peripheral smear review confirmed marked eosinophilia (75%) with very few (1%) circulating lymphoblasts (panel A; Wright-Giemsa, original magnification ×100), positive by flow cytometry for CD10 (bright) and CD19 (panel B), along with CD34, TDT, CD22, cCD79a, HLA-DR, CD9, CD58, and CD123. Bone marrow examination showed 70% to 80% involvement by B-lymphoblastic leukemia/lymphoma (B-ALL), with aspirate demonstrating sheets of blasts admixed with eosinophils/eosinophilic precursors (panel C; Wright-Giemsa, original magnification ×100). The core biopsy showed 70% to 80% B-ALL lymphoblasts (panel E; hematoxylin and eosin, original magnification ×40), which are TDT positive (panel F; TDT, original magnification ×40), along with admixed eosinophils/eosinophilic precursors. The cytogenetic study showed high hyperdiploid karyotype: 52,XY,+X,+4,+9,+14,+21,+21 (panel D). The most common translocation t(5;14) (q31;q32) associated with B-ALL cases with hypereosinophilia, as well as relatively less common recurrent abnormalities such as translocation t(7;12)(q22;p13) and deletions involving 5q, 7q, were not identified.
The current study highlights the need for high suspicion of B-ALL and bone marrow examination in a hypereosinophilia case presenting with very few or no circulating lymphoblasts. The hyperdiploid karyotype is an example of cytogenetic diversity of B-ALL cases associated with hypereosinophilia.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal