Introduction:
Paroxysmal nocturnal hemoglobinuria (PNH) often presents as hemolysis and/or bone marrow failure. Flow cytometric testing can accurately detect PNH. However, the long term studies on PNH clone size and how it relates to clinical course are few. We sought to understand how PNH clone size correlates with clinical course over time and the impacts on clone size with different treatments. Here we report long term clone size monitoring and clinical data of 57 patients with PNH in a single intuition.
Methods:
High sensitivity PNH flow cytometry (0.01% limit of detection) was performed with FLAER-FITC, CD64-PE, CD14-ECD, CD15-PC5, CD24-AA7500, CD45-KO for neutrophils & monocytes; CD59-PE and CD235a-AA750 for RBCs.
Retrospective analysis was done in the positive PNH cases from 2008-2019 at OHSU. Total 173 cases for 57 patients; including 27 females and 30 males, 52 adults and 5 pediatrics, with a mean age of 45 (range 9-78). We also reviewed results of serum LDH, bone marrow biopsies and molecular/cytogenetics of these patients. Among of these patients, 18 patients (11 females and 7 males, mean age 49.33, age range 29-73) with long term (at least over 4 years) follow-up have more than 3 PNH tests. Besides PNH clone on RBC and PMN, we also reviewed results of WBC count (x103/ul), Hb (g/dL), PLT (x103/ul) serum LDH (U/L), bone marrow biopsy reports and molecular/cytogenetics findings in these patients.
Results:
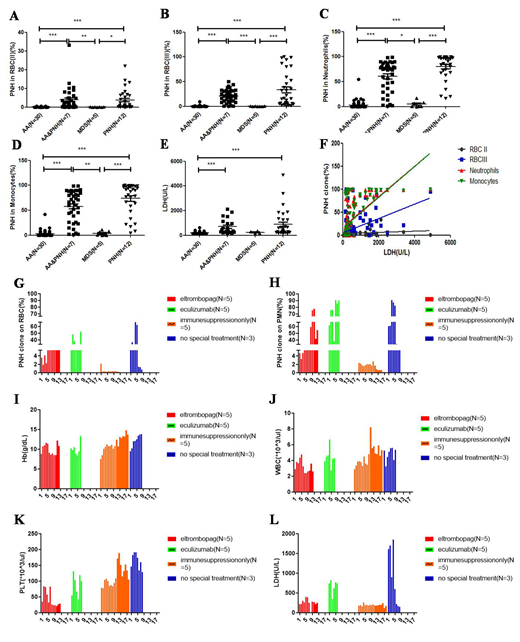
Among 57 patients, there are 30 aplastic anemia (AA) patients (53.63%), 7 AA patients progressing to PNH (AA&PNH, 12.28%), 5 myelodysplastic syndromes (MDS, 8.77%), 12 PNH patients (21.05%), 1 pancytopenia, 1 autoimmune disease, 1 thrombosis. The diagnosis of AA and MDS were confirmed by bone marrow biopsy and molecular/cytogenetics. Significantly higher levels of all PNH clones were observed in PNH and AA/ PNH, compared to AA (all P <0.001) and MDS (all P<0.05) shown in Figure A-D. LDH was higher in PNH and AA/PNH than AA and MDS groups (P<0.001, Figure E). LDH demonstrated positive correlation with PNH clone size in RBC-type-III, neutrophils and monocytes (all P<0.0001, R= 0.4447, 0.5469, 0.5711, respectively, Figure F). No correlation was observed between LDH and RBC-type-II.
Long term (4-11 years ) follow up include 18 patients were divided into 4 groups: 5 AA treated with immunosuppressant only, 5 AA treated with immunosuppressants and/or eltrombopag, 5 classic PNH or AA that progressed to PNH treated with immunosuppressants and/or eculizumab, and 3 PNH with observation and supplements only. The study showed immunosuppression only has lowest PNH clone size for both RBC and WBC (Figure G-H). As for the Hb and WBC count, there were no statistics differences among 4 groups (Figure I-J). Decreased PLT was detected in eltrombopag group (Figure K). Significantly, increased LDH was observed in the observation/supplement group (Figure L). Interestingly, all these 3 patients without special treatment have high PNH clones and LDH from diagnosis to now over 10 years. Despite receiving basic supportive care, the patients' clinical courses have been stable with only supplementation of vitamin B12 and Folic Acid.
Conclusions: Positive PNH test was most frequently seen in AA patients. AA has lower PNH clone size and LDH than those of PNH patients or AA progressed to PNH patients. For all patients, PNH population showed positive correlation with LDH. Our study suggest that it is necessary to follow PNH clone size, as this may impact the decision of when to start therapy with what agents.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal