Background: Hematopoietic cell transplantation (HCT) has curative potential in sickle cell disease (SCD). A reduced intensity haploidentical bone marrow transplant (haplo-BMT) platform piloted by investigators at Johns Hopkins, addressed key barriers in HCT for SCD, donor availability and toxicity, but had a graft rejection rate of 43%. (Blood. 2012;120(22):4285-4291). Subsequently, a Vanderbilt University Medical Center supported multi-institution learning collaborative with London, France and United States was developed in 2013 with the objective of reducing this graft rejection rate. Evolution of this haplo-BMT platform with the addition of only thiotepa, resulted in a reduction in the graft rejection rate to 7% (1 of 15), an event free survival (EFS) of 93% (14 of 15), > 95% stable donor engraftment at 6 months and 100% overall survival (Biol Blood Marrow Transplant. 2019 Jun;25(6):1197-1209). Based on the preliminary data from the learning collaborative, we initiated an NIH sponsored BMT CTN, dual-strata, phase II, multi-center prospective clinical trial, (clinicaltrials.gov # NCT03263559) to estimate event free survival (EFS) at 2 years in children with neurological morbidity and adults with severe SCD.
Study Design and Methods: Eligibility: Patients are stratified into 2 groups: (1) children with SCD (Hb SS or Sβ+ Thalassemia) between 5.00 - 14.99 years of age with central nervous system (CNS) disease (stroke, elevated transcranial Doppler (TCD) with evidence of intracranial vasculopathy; silent cerebral infarction) and (2) adults with severe SCD (Hb SS, SC, Sβ° thalassemia, Sβ+ Thalassemia, SD, S-OArab), between 15.00 - 45.99 years of age who have had a stroke, recurrent ACS, recurrent vaso-occlusive pain episodes, chronic transfusions to prevent sickle complications and tricuspid valve regurgitant jet velocity (TRJV) ≥2.7 m/sec. Participants must have an HLA haploidentical first degree relative donor with 2, 3, or 4 (out of 8) HLA-mismatches who is willing and able to donate bone marrow. Those with an HLA-matched sibling are excluded. Primary objective is to estimate EFS at 2 years after haplo-BMT in patients with SCD enrolled in each stratum. Secondary objectives include determining the effect of haplo-BMT on clinical and laboratory manifestations of SCD by 2 years post-transplant and determining the incidence of other transplant-related outcomes. A key secondary analysis will be central adjudication of CNS progression in children and adults with evidence of previous CNS injury.
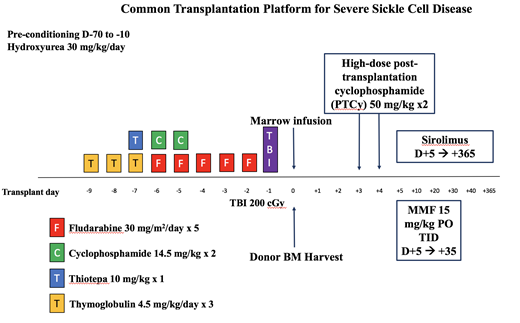
Treatment Description: Preconditioning with hydroxyurea 30mg/kg daily (Day -70 to Day -10). The conditioning regimen includes: Thymoglobulin (rATG) (0.5mg/kg on Day -9, 2mg/kg on Day -8, Day -7), Thiotepa 10mg/kg on Day -7, Fludarabine (30mg/m2 on Day -6 to Day -2), Cyclophosphamide 14.5mg/kg on Day -6 and Day -5, and TBI 200cGy on Day -1. Day 0 is the day of infusion with non T-cell depleted bone marrow. Cyclophosphamide 50 mg/kg and Mesna 40mg/kg is given on Days +3 and +4, and GVHD prophylaxis (sirolimus and mycophenolate mofetil) begin on Day +5 (Figure).
Study Accrual and Endpoints: The target sample size is 40 patients enrolled and treated in each stratum; if the stopping rule for graft failure is triggered within the first 12 evaluable participants in either stratum using the 200cGy dose of TBI and the DSMB and sponsor approve the pre-defined switch in conditioning regimen, then accrual for that strata will restart under the modified conditioning regimen with 400 cGy TBI. The estimated accrual period is 4 years. The rate of overall mortality by Day 180 after starting hydroxyurea therapy pre-transplant, acute grade III-IV GVHD at 100 days, and severe chronic GVHD at 18 months post-transplant will be monitored by a sequential probability ratio test (SPRT) for censored exponential data for each of these. Graft failure at 100 days post-transplant will be monitored by using a SPRT for binary data.
Conclusion: This NIH sponsored BMTCTN phase II trial of HLA-haploidentical HCT is active at 30 BMT CTN sites. This study will determine if a modulated conditioning regimen has adequate donor engraftment, with acceptable risks of transplant-related morbidity and mortality to support a future comparative clinical trial in SCD.
Walters:AllCells, Inc: Consultancy; TruCode: Consultancy; Editas Medicine: Consultancy. Brodsky:Achillion: Research Funding; Alexion: Membership on an entity's Board of Directors or advisory committees, Other: Grant funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal