Background: Although frailty influences outcomes in hematologic oncology, little is known about the feasibility and impact of embedded geriatric consultation for frail older adults with blood cancers.
Methods: From February of 2015 until May 2018, all patients aged 75 and older presenting for initial consultation for hematologic malignancy at the Dana-Farber Cancer Institute (DFCI) were approached for geriatric screening by a trained clinic assistant. In a 15-minute interview, the assistant used two parallel methods-the phenotype approach (Fried, J Geront A Biol Sci Med Sci, 2001) and the cumulative deficit approach (Rockwood, J Geront A Biol Sci Med Sci, 2007) -to characterize patients as "frail," "pre-frail," or "robust." Patients determined to be frail of prefrail on at least one of the two screening methods who had a scheduled oncology follow-up at DFCI were then randomized to have tandem consultation with an embedded board-certified geriatrician; the schema used an unbalanced allocation design powered to detect differences in one-year overall survival. Patients were followed for hospitalizations and emergency department visits in the first six months after enrollment, documented discussions about goals of care at the end of life during the first year by any DFCI outpatient provider (resuscitation status, hospice, or preferred location for dying using criteria from Mack, Ann Intern Med, 2012), and one-year overall survival. We also undertook a survey of the 65 oncologists and physician extenders who had utilized geriatric services, asking them about consultation usefulness (on a Likert scale where 1= "least" and 5 = "most" useful) for evaluating cognition, informing treatment decisions, connecting patients to resources, and managing non-oncologic comorbidities. We conducted pairwise analyses using McNemar's test to identify the most useful services.
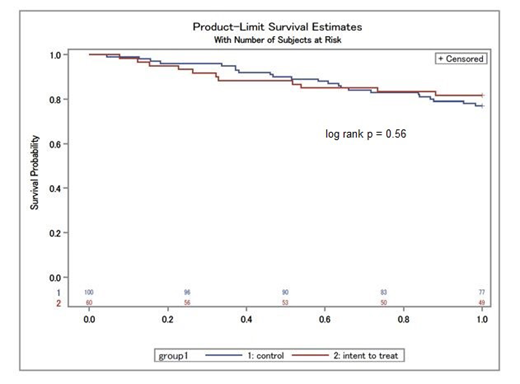
Results: Of 186 patients approached, 160 enrolled, with 60 randomized to geriatric consultation and 100 to usual care. Mean age was 80.4 years, 65% were male, and 30% were initially seen in the MDS/leukemia clinic, 31% in the lymphoma clinic and 39% in the myeloma clinic. Of those randomized to geriatric consultation, 48 (80%) completed at least one visit with an embedded geriatrician (95% CI [68%, 88%]). Among the 12 who did not, 3 died before the scheduled consultation, 6 ultimately did not to return to DFCI, and 3 cancelled their geriatric appointments. In an intent-to-treat analysis, patients assigned to consultation were no less likely to die within one year (Figure; HR 0.99, 95% CI [0.58, 1.68]). Results were also not significant in as-treated analysis (HR 0.87, 95% CI [0.49, 1.55]).
In negative binomial regression analysis, patients assigned to geriatric consultation had modestly fewer unplanned hospitalizations and emergency room visits than those randomized to usual care, but the results were not significant. The odds of having a documented discussion about goals of care for patients randomized to geriatric co-management were 2.66 (95% CI [0.95, 7.41]; p=.06) times versus for those receiving usual care; for those who actually completed a geriatrician visit, they were 3.07 (95% CI [1.06, 8.82]; p=.04).
Of 65 providers surveyed, 37 responded (57%). Mean responses in the "5 = most useful" category for each question were as follows: managing non-oncologic comorbidities 60%, connecting patients to resources 57%, evaluating cognition 49%, and informing treatment decisions 34%. McNemar's tests revealed that managing non-oncologic comorbidities was no more likely to be considered "most useful" than connecting patients to resources (p=.48) and evaluating cognition (p=.06) but more likely than informing treatment decisions (p=.01). Connecting patients to resources was no more likely to be considered "most useful" than evaluating cognition (p=.37) but more likely than informing treatment decisions (p=.04).
Conclusion: Embedded geriatric consultation for frail and pre-frail older adults with blood cancers is feasible but may not affect acute care utilization or survival in the first year. In contrast, consultation likely has a substantial impact on the timeliness of discussions about goals of care at the end of life. Oncology providers report that embedded geriatric consultation is useful among many care domains, but most helpful for managing comorbidities and connecting patients to resources.
Stone:AbbVie, Actinium, Agios, Argenx, Arog, Astellas, AstraZeneca, Biolinerx, Celgene, Cornerstone Biopharma, Fujifilm, Jazz Pharmaceuticals, Amgen, Ono, Orsenix, Otsuka, Merck, Novartis, Pfizer, Sumitomo, Trovagene: Consultancy; Argenx, Celgene, Takeda Oncology: Other: Data and Safety Monitoring Board/Committee: ; Novartis, Agios, Arog: Research Funding. Soiffer:Kiadis: Other: supervisory board; Gilead, Mana therapeutic, Cugene, Jazz: Consultancy; Juno, kiadis: Membership on an entity's Board of Directors or advisory committees, Other: DSMB; Jazz: Consultancy; Cugene: Consultancy; Mana therapeutic: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal