Background. The end phase or metamorphosis is one of the remaining challenges of chronic myeloid leukemia (CML) management. Blast crisis (BC) is a late marker. Earlier diagnosis may improve outcome. The detection of additional chromosomal abnormalities (ACA) at low blast levels might allow earlier treatment when outcome is better.
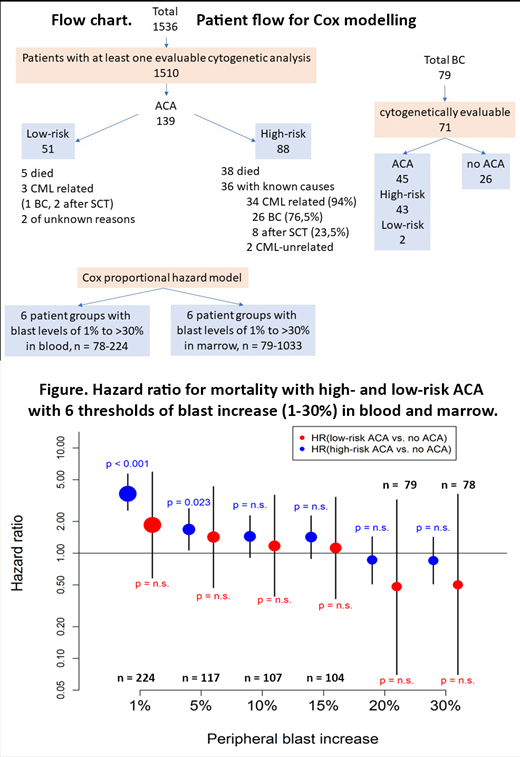
Methods. We made use of 1536 Ph+CML-patients in chronic phase followed in the randomized CML study IV (Hehlmann et al, Leukemia 2017) for a median of 8.6 years. 1510 cytogenetically evaluable patients were analyzed for ACA and blast increase (Flow chart). According to impact on survival ACA were grouped into high-risk (+ 8; +Ph; i(17q); +17; +19 +21; 3q26; 11q23; -7; complex) and low-risk (all other). Prognosis with +8 alone was clearly better than with +8 accompanied by further abnormalities, but still worse than with low-risk ACA. +8 alone was therefore included in the high-risk group. The presence of high- and low-risk ACA was linked to 6 thresholds of blast increase (1%, 5%, 10%, 15%, 20%, and 30%) in a Cox proportional hazards model.
Results. 139 patients (9.2%) displayed ACA at any time before BC diagnosis, 88 (5.8%) had high-risk and 51 (3.4%) low-risk ACA. ACA emerged after a median of 17 (0-133) months. 79 patients developed BC. 43 (61%) of 71 cytogenetically evaluable patients with BC had high-risk ACA. 3-year survival after emergence of high-risk ACA was 48%, after emergence of low-risk ACA 92%. At low blast levels (1-15%), high-risk ACA showed an increased hazard to die (ratios: 3.66 in blood; 6.84 in marrow) compared to no ACA in contrast to low-risk ACA. This effect was not observed anymore at blast increases to 20-30% (Figure). 38 patients with high-risk ACA died, 36 with known causes of death which were almost exclusively BC (n=26, 72%) and progression-related transplantation (n=8, 22%). Only 2 patients died of CML-unrelated causes.
Conclusions. High-risk ACA herald death by BC already at low blast levels and may help to define CML end phase in a subgroup of patients at an earlier time than is possible with current blast thresholds. Cytogenetic monitoring is indicated when signs of progression surface and response to therapy is unsatisfactory. More intensive therapy may be indicated at emergence of high-risk ACA.
Hehlmann:Novartis: Research Funding. Haferlach:MLL Munich Leukemia Laboratory: Employment, Equity Ownership. Fabarius:Novartis: Research Funding. Krause:Siemens: Research Funding; Takeda: Honoraria; MSD: Honoraria; Gilead: Other: travel; Celgene Corporation: Other: Travel. Baerlocher:Novartis: Research Funding. Burchert:Novartis: Research Funding. Brümmendorf:Novartis: Consultancy, Research Funding; Janssen: Consultancy; Merck: Consultancy; Ariad: Consultancy; Pfizer: Consultancy, Research Funding; University Hospital of the RWTH Aachen: Employment. Hochhaus:Pfizer: Research Funding; Novartis: Research Funding; BMS: Research Funding; Incyte: Research Funding; MSD: Research Funding. Saussele:BMS: Honoraria, Research Funding; Incyte: Honoraria, Research Funding; Pfizer: Honoraria; Novartis: Honoraria, Research Funding. Baccarani:Novartis: Consultancy, Speakers Bureau; Incyte: Consultancy, Speakers Bureau; Takeda: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal