Introduction: Patients with absolute neutrophil count (ANC) <1500 x10^9/L are frequently referred to Pediatric Hematology Oncology. Scant literature exists on outcomes and interventions for isolated neutropenia. We hypothesize that most patients will have resolved neutropenia without the need for an intervention from Pediatric Hematology Oncology.
Methods: We performed a five-year IRB-approved, retrospective chart review of patients referred to a Pediatric Hematology-Oncology clinic for isolated neutropenia. Patients were excluded if they also had anemia or thrombocytopenia at the time of the referral. Degree of neutropenia was categorized: 1) at the time of referral, 2) at the lowest value, and 3) at the current ANC as Mild: 1.001-1.500 x109/L, Moderate: 0.501-1.000 x109/L, Severe: 0.201-0.5 x109/L, or Very Severe ≤0.2 x109/L. Descriptive statistics and odds ratios were performed.
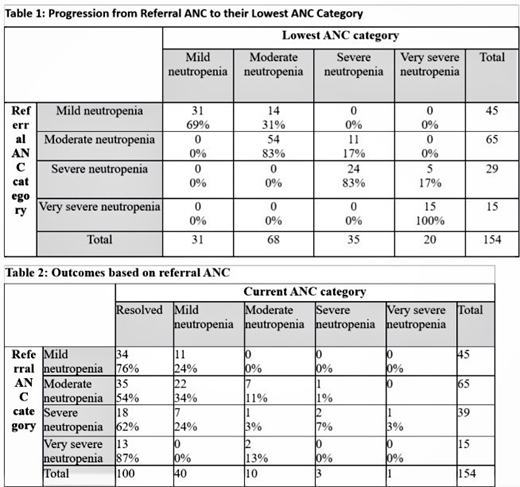
Results: Among 154 patients referred with isolated neutropenia over five years, 45 (29%) had mild neutropenia, 65 (42%) had moderate neutropenia, 29 (19%) had severe neutropenia, and 15 (10%) had very severe neutropenia. Only 29 (19%) patients progressed to a lower ANC category than their referral ANC category. At a median follow-up of 12 months, 101 (66%) patients had resolved neutropenia, 40 (26%) patients had mild, ten (6%) patients had moderate, three patients had severe, and one patient had very severe neutropenia. Most patients (54%) were not identified with a specific diagnosis. The most common diagnoses included viral suppression (16%), autoimmune neutropenia (14%) and drug induced neutropenia (8%). The most common medications reported as responsible for neutropenia were either anti-epileptic medications or immunosuppressant medications. No patients were diagnosed with a malignancy. Black patients had a 3.5 times higher odds of having persistent, mild, undiagnosed neutropenia which, for some patients, may be benign ethnic neutropenia. Seven (4.5%) patients received G-CSF therapy. Five patients were either managed by a Rheumatologist or an Immunologist. Finally, there were 16 hospitalizations that occurred in 10 patients for a prevalence of one admission for every 21 patient years. The most common admission diagnosis was febrile neutropenia without subsequent bacteremia (n=13).
Conclusion: Most pediatric patients referred for isolated neutropenia do not progress, develop leukemia, or require sub-specialty interventions. Hospitalization of patients referred for isolated neutropenia is rare as is bacteremia. This study provides important outcome data that can improve our counseling of pediatric patients identified with isolated neutropenia.
Howard:Novartis: Consultancy. Lebensburger:Novartis: Consultancy; Pfizer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal