Immune checkpoint inhibitors such as CTLA-4 and PD-1 inhibitors mediate T-cell induced tumor cell destruction by blocking malignant cells' ability to negatively regulate T cell activity. In addition to its anti-tumor effect, checkpoint inhibition can lead to loss of maintenance of self-tolerance, leading to immune-mediated adverse events (irAEs). These events can affect any organ, with pneumonitis, hepatitis, and colitis among the most commonly reported events. A rare and life-threatening reported side effect is cytokine release syndrome (CRS).
CRS is a systemic inflammatory response described in a number of cancer immunotherapies, including CAR T-cell and bispecific T-cell engagers (BiTEs). The primary pathophysiology involves activation of bystander immune and non-immune cells (such as endothelial cells) leading to a massive release of inflammatory cytokines. CRS can present as a benign, flu-like syndrome, or as an overwhelming, life-threatening systemic disease characterized by hypotension, capillary leakage, disseminated intravascular coagulopathy, and multi-organ failure. IL-6 appears to play a critical role in CRS through activation of the complement and coagulation cascade. The IL-6 inhibitor tocilizumab is the only FDA-approved treatment for CRS.
There have been several reported cases of checkpoint inhibitor-induced CRS reported in the literature, including a 25-year-old patient with Hodgkin's Lymphoma (Zhao L, et al. Immunotherapy 2018) and a 29-year-old patient with sarcoma (Rotz SJ, et al. Pediatr Blood Cancer 2017). CRS developed in these cases after the first and second doses of nivolumab, respectively. We now present an additional rare case of CRS from nivolumab therapy that occurred months after initiation of treatment.
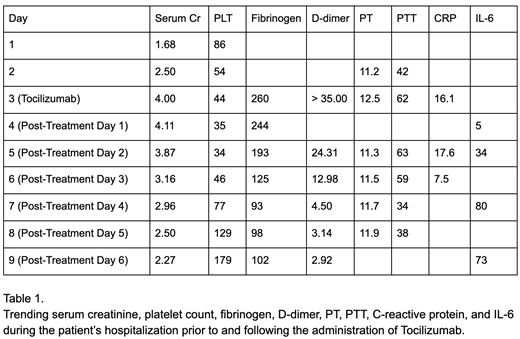
We present a 71-year-old male with stage IV melanoma on cycle 17 of nivolumab with a partial response who was admitted to our institution with altered mental status, hypotension, tachycardia, fever up to 104.9°F, and hypoxia requiring BiPAP. On physical exam, he was noted to have a grade 3 maculopapular rash. Lab work on presentation was notable for serum creatinine of 1.68, platelet count of 86, d-dimer > 35, and CRP of 16.1.
He was started on vancomycin and piperacillin-tazobactam for suspected sepsis. After 24 hours with no improvement, he was started on 1 mg/kg methylprednisolone due to growing concern that symptoms were immune-mediated. After another 24 hours with no improvement, tocilizumab was administered for the suspicion of CRS. The patient's clinical status began to improve within one hour of treatment with resolution of fever and hypotension, as well as improvement in hypoxia and mental status. Over the next several days, his platelet count and kidney function significantly improved as well. Decreased CRP levels suggesting a blunting of his inflammatory response, and increased IL-6 levels from IL-6 receptor blockade were seen as well. He was discharged from the hospital in good condition on day 6 post-treatment after stabilization of unrelated comorbid conditions, and followed up one week after discharge at his baseline level of function. He unfortunately developed another episode of CRS six weeks after discharge and passed away despite attempted treatment with tocilizumab.
CRS remains a rare, potentially life-threatening condition that requires early diagnosis and management. Although initial investigations may point to more common conditions such as infection and sepsis, a low threshold for consideration of irAEs and CRS should exist where the clinical picture warrants. There are likely many more cases in which the diagnosis is missed and appropriate treatment not given due to lack of clinical awareness. Had our patient's symptoms not been clinically recognized as CRS by the inpatient hematology team, his condition would have likely been terminal due to the presumed diagnosis of sepsis. Physician education, particularly in the ED and ICU, early consultation, and prompt implementation of specific testing and treatment with tocilizumab can lead to significantly improved outcomes as our case shows. The unfortunate second CRS event and failure to repeatedly respond to tocilizumab with his second episode reinforces the need for continued research for additional treatment options for CRS, especially in recurrent cases.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal