INTRODUCTION
Myeloma cast nephropathy (CN) is the most common form of monoclonal immunoglobulin-mediated kidney disease, resulting from the precipitation of excessive amounts of monoclonal serum free light chains (sFLC) and causing around 70% of the cases of dialysis-dependent renal failure in multiple myeloma (MM)(Heher et al. 2013; Nasr et al. 2012; Sanders et al. 1991). In patients with acute renal failure, the finding of a high sFLC concentration with an abnormal sFLC ratio raises the clinical suspicion of CN (Hutchison et al. 2011). Although the histopathologic diagnosis of CN is established by renal biopsy, in routine clinical practice, the diagnostic yield of this procedure is often outweighed by the urgent need of anti-myeloma treatment and the risk of procedure-related complications. Recruitment of patients with CN into clinical trials is challenging and therefore real-world data on clinically suspected CN are necessary to understand the clinical characteristics, treatment and prognosis of these patients (Bridoux et al. 2017; Hutchison et al. 2019).
METHODS
We searched the population-based Danish Multiple Myeloma Registry for patients diagnosed with MM according to the International Myeloma Working Group criteria between 1st of January 2013 and 31st of December 2017 with a serum creatinine concentration of 200 µg/L or higher and a sFLC concentration of 1000 mg/L or higher at diagnosis. We conducted a retrospective patient chart review in eight Danish centers and assessed baseline characteristics, biopsy results, and overall survival. Anti-myeloma treatment, sFLC levels and renal function were registered during the first 12 months after MM diagnosis.
RESULTS
We identified 181 patients (176 with accessible clinical records). The median age was 72 years, the median serum creatinine was 384 µg/L, the median involved sFLC concentration was 5960 mg/L and dialysis dependent renal failure was present in 35%. Pre-myeloma estimated glomerular filtration rate (eGFR) was available in 80%, the median eGFR was 66 ml/min/1.73 m2. A kidney biopsy was carried out in 21% of patients and showed CN in 70% of cases. The median time from first sFLC measurement to initiation of therapy was 4 days.
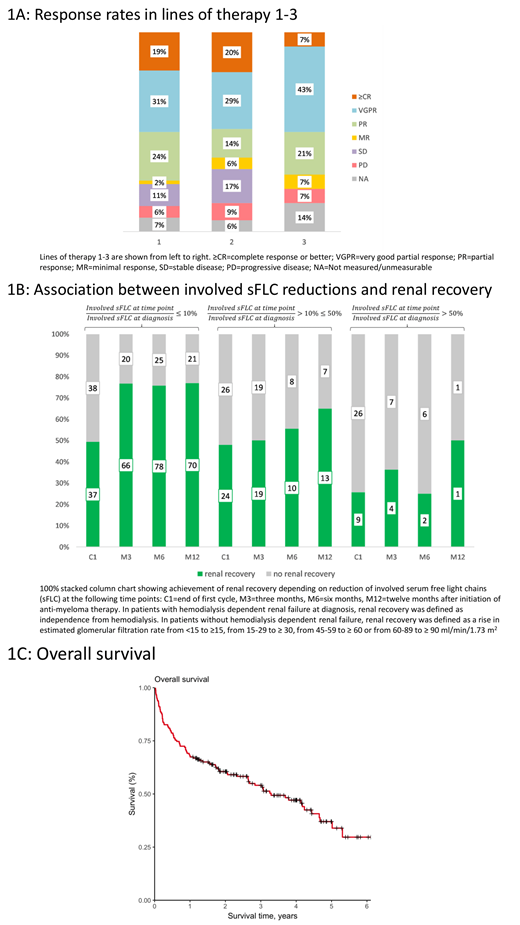
The number of lines of therapy ranged between zero and six. 173 patients received one, 35 patients received two and 14 patients received three lines of therapy during the first 12 months from diagnosis. High-dose melphalan with autologous stem cell transplantation (HDT-ASCT) was carried out in 45 (26%) patients. Bortezomib was administered as part of the first-line regimen in 163 (94%) patients. The most common first-line regimens were bortezomib-dexamethasone (n=67) and cyclophosphamide-bortezomib-dexamethasone (n=46). The first line of therapy resulted in very good partial response or better in 50% (Figure 1A), but was discontinued due to death, toxicity or progressive disease in 38% of patients.
Dialysis dependency, eGFR and involved sFLC concentration were assessed at the end of the first cycle, at three months, six months and 12 months after initiation of therapy. At all these time points, achievement of renal recovery was associated with the magnitude of reduction of involved sFLC (Figure 1B). The median overall survival was 3.3 years (Figure 1C). At 12 months after diagnosis, 68% of patients were alive and 15% were dialysis dependent. Reduction of the initial involved sFLC concentration to ≤ 10% at three months was strongly associated with longer OS in a multivariate cox regression analysis adjusted for age and HDT-ASCT; hazard ratio 0.42, p=0.003.
CONCLUSION
In conclusion, we assessed a population-based cohort of newly diagnosed MM patients presenting with a serum creatinine of 200 µg/L or higher together with a sFLC of 1000 mg/L or higher. Although CN could have been clinically suspected in these cases, a kidney biopsy was only performed in one fifth of the population. Bortezomib-based therapy was initiated quickly and resulted in deep responses in most patients. Approximately one third of patients died within a year from MM diagnosis. Achievement of early and deep reduction in involved sFLC resulted in longer OS.
Szabo:Janssen: Consultancy. Vangsted:Takeda: Membership on an entity's Board of Directors or advisory committees; Jansen: Honoraria; Celgene: Honoraria; Sanofi: Membership on an entity's Board of Directors or advisory committees; Oncopeptides: Membership on an entity's Board of Directors or advisory committees. Plesner:Celgene: Consultancy; AbbVie: Consultancy; Genmab: Consultancy; Oncopeptides: Consultancy; Takeda: Consultancy; Janssen: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal