Introduction: Peripheral T-cell lymphomas (PTCL) are a heterogeneous group of mature T-cell neoplasms with aggressive behavior and dismal outcomes. Anthracycline-based chemotherapy is commonly used upfront; hematopoietic stem-cell transplantation (HSCT) is employed as consolidation by some groups. Refractory/relapsed cases (R/R) have a median survival of less than 6 months. Our objective was to analyze the outcomes of all consecutive PTCLs diagnosed and treated in a single center during 16 years according to histological subtype, disease phase (first line and R/R) and treatment strategies.
Patients and methods: All adult PTCL patients referred to our center between 2003 and 2019 were included. All cases were locally diagnosed based on the current WHO classification by an expert hemato-pathologist. Initial clinical features, treatment and outcomes were analyzed, as well as salvage strategies.
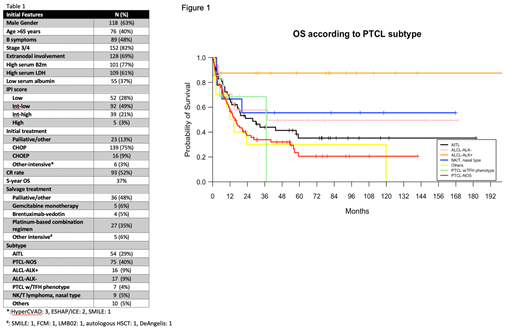
Results: A total of 188 patients were included (118 male, 70 female; median age 62 years). Median OS was 22.7 months, with a median follow up of 54 months. Histological subtypes, initial features, response to treatment and survival are detailed in table 1. Briefly, most cases were diagnosed at advanced stages, with extranodal involvement in 69% and elevated beta-2 microglobulin (B2m) in 77%; half had B symptoms. OS according to different subtypes is shown in figure 1. Of note, anaplastic large cell lymphoma (ALCL)-ALK+ patients had a 5-year OS of 88%. Interestingly, fifteen patients had circulating lymphoma cells (12 PTCL not otherwise specified [NOS], 2 hepatosplenic lymphoma and 1 angioimmunoblastic lymphoma [AITL]), with no impact on outcome. PTCL-NOS was the most prevalent subtype (40%) followed by AITL; unexpectedly, the proportion of PTCL-NOS cases increased while AITL cases decreased after 2008. Seven cases belonging to the recently recognized nodal PTCL with T follicular helper (TFH) phenotype were observed, with baseline characteristics and outcome similar to other PTCLs. IPI score index stratified patients into 4 groups with 24-month OS of 71%, 55%, 42% and 16% for low, int-low, int-high and high risk patients, respectively (P=.049). Only B2m and IPI score maintained independent significance for OS (HR= 3.2 and 1.8, respectively, P<.01) in a multivariate analysis that also included histologic subtype and frontline treatment. Most patients were treated with CHOP (75%), although other regimens were increasingly used in recent years, including CHOEP (9%). Young (<65 years) PTCL-NOS patients had a better outcome when treated with CHOEP compared to CHOP (24-month OS of 100% vs. 37%, P=.04); this difference was not noted in ALCL-ALK- and in AITL cases. Twenty-three patients (21% of transplant-eligible cases) underwent HSCT (18 autologous, 5 allogeneic), mostly (16/23) in first remission. As expected, patients not responding to frontline therapy or relapsing after CR showed a dismal outcome (median OS of 4.1 months from R/R date). Intensive platinum-based salvage treatments (26 cases) led to a median OS from relapse of only 6 months. In contrast, single-drug Gemcitabine at first relapse showed a median OS 17.4 months in 5 elderly patients. Of 76 R/R transplant eligible patients, only 7 underwent HSCT(4 allogeneic, 3 autologous), with a 5-year OS of 86%. Eight patients (4 AITL, 4 ALCL) received Brentuximab-Vedotin (BV) at first or later relapse, with improved outcomes compared to other regimes (24-month OS of 63% vs. 22%, P=.03).
Conclusion: Initial features, treatments and outcomes for PTCL have not significantly changed in a 16-year period. Only a minority of cases underwent HSCT or received new agents. Ideal salvage regimens are not defined and, in our experience, single agent Gemcitabine or BV performed better than more aggressive combinations. Although promising new drugs have been recently approved for PTCL, their impact on outcome is still not clear. Recent progresses in molecular characterization of the disease may translate into better outcomes through prospective collaborative efforts in the near future.
Silva:Gilead Sciences: Consultancy, Other: Travel support, Research Funding; Janssen Cilag: Consultancy, Other: Travel support; Abbvie: Consultancy, Other: Travel support; Celgene: Consultancy; Roche: Consultancy, Other: Travel support.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal