Introduction. Presence of measurable by flow cytometry (FC) residual disease (MRD) is a well-known risk factor in AML patients (pts), which is associated with adverse prognosis. The main idea in MRD by FC is searching for leukemia-associated immunophenotype (LAIP) which is based on «different from normal (DfN) approach». DfN approach allows to capture any immuphenotypic (IP) shifts during the therapy. LAIP may change in 16-91% AML cases. There are some ELN recommendations for monoclonal antibodies (mAbs) which allows todetect "mandatory (most frequent)" aberrations. But each laboratory uses its own tactics for MRD detection, taking into account the capabilities and equipment, and approved standardized panel still does not yet exist.
Aim. To find the most common and adverse IP aberrations of blast cells in the onset of AML, and to determine the frequency of IP shifts during treatment and in relapse.
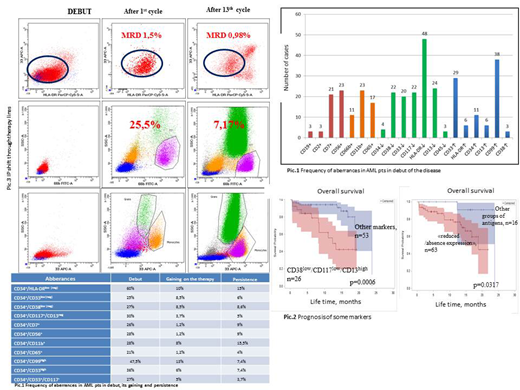
Patients and methods. From March 2016 to February 2018 71 newly diagnosed AML (18-79 y.o.) pts were included in the initial LAIP (before any treatment) detection in hematology department of National Research Center for hematology, Moscow, Russia. MRD was detected in bone marrows by FC with BD FACS Canto II. The standard panel included mAbs against CD19, CD7, CD2, CD38, CD65, CD66b, CD99 (FITC); CD56, CD15, CD11b, CD13 (PE); CD33 (APC); HLA-DR, CD14, CD16, CD117 (PerCP-Cy 5.5); CD45 (APC-H7) and CD34 (PE-Cy7). MRD was determined after 1st and 2nd treatment course and in relapse. Pts received different treatment strategy due to age, comorbid status, severe infectious complications and type of AML. Most common for 80% of pts was induction course «7+3». Next cycles differed by intensity. The threshold value of 0.01% was estimated for long-term prognosis in our research.
Results. The distribution of aberrations of blasts in the AML onset is shown in pic. 1. The most common aberration was "reduced /absence expression": in 60% of pts it was observed in the combination CD34+/HLA-DRlow (HLA-DR-). The appearance of this aberration and its preservation during the course of therapy were also more common (10% - 15%) than others (pic 1).
When analyzing the results of long-term survival, it was shown that low expression of CD38 and/or CD117, as well as increased expression of CD13 in combination with CD34+ on blast cells in AML onset, is associated with bad prognosis (pic.2). CD117 and CD38low are the earliest markers of progenitor cells and show the region for identifying stem cells and leukemic stem cell. When analyzing the remaining groups of aberrant combinations (overexpression, asynchronous and non-linear expression), no correlation with the long-term prognosis was revealed.
From 15 relapses of AML, the change of the primary LAIP was detected in 40%. Of the 7 refractory AML pts, the change of primary LAIP was detected in 57%. Complete replacement of the primary LAIP - in 18% from those with relapse and refractoriness (pic 3).
Conclusion. The immunophenotyping shifts in AML pts is a very common phenomenon. In our study 60% of LAIP in relapse remained the same and 43% was the identical in refractory pts. LAIP shifts during chemotherapy reflects the biology of the tumor and its low sensitivity to therapy, but eventually leads to relapse development. To cover all potential changes in the IP and early suspect the relapse development to change the tactics of therapy, it is necessary to use the complex standardized mAbs panel, which allows determining as many aberrancies, as possible.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal