
INTRODUCTION
Secondary Acute Myeloid Leukemia (s-AML) evolves from a previous hematopoietic clonal disease such as Myelodysplastic Syndromes (MDS/AML), myeloproliferative neoplasia (NPM/AML), medullary insufficiencies - aplastic anemia - (AA/AML) or exposure to chemo or radiotherapy (t-AML). The objective of this work is to describe and highlight the demographic, pathophysiologic and clinical-therapeutic characteristics of s-AML patients compared with p-AML.
METHODS
This is a retrospective cohort study based on the casuistry from 34 reference centers in Latin America during a period of 10 years (JAN10'-MAY19'). Patients ≥18 years old with primary AML, excluding the promyelocytic subtype (p-AML), and s-AML were admitted. Age, gender, performance status, comorbidity, cytogenetics, mutations, AML subtypes, extramedullary compromise, treatments and overall survival (OS) were analyzed. Statistically, Graph Pad Prism version 5.00 and, SPSS version 17 were used.
RESULTS
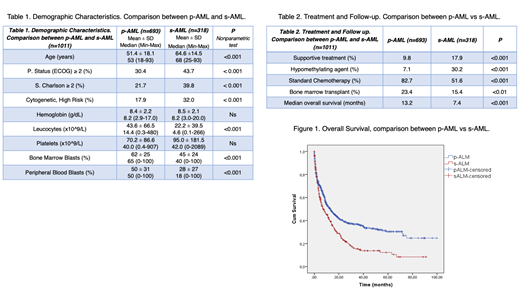
One thousand eleven patients with newly diagnosed AML were recruited, 693 (68.5%) corresponded to p-AML and 318 (31.5%) to s-AML. The demographic differences between p-AML and s-AML are shown on Table 1. Subtypes of s-AML: t-AML (18.5%), MDS/AML (58.2%), NMP/AML (13.5%), AA/AML (5.7%) and others s-AML (4.1%). Global median age was 58 years (R 18-93) and male 52%. Extramedullary compromise in CNS (3.2%) and other organs (5.5%). Seven hundred ninety-three cytogenetic studies were evaluable (based on MRC classification): High (22.3%), Intermediate (68.3%) and Low Risk (9.3%). FLT3 mutation was more frequently found in p-AML. In s-AML, the multivariate study showed short overall survival associated with ECOG ≥2 (HR:2.0), white blood count ≥ 50x109/L at diagnosis (HR:1.9), poor risk karyotype (HR:1.6) and age over 60 years (HR:1.5). At least, 883 patients received treatment (Table 2). During this study period, 211 patients (21%) were transplanted; 49 (23%) were s-AML; histoidentical related donor (46%), haploidentical (39%), non-related (8%) and autologous (7%). The median survival for all AML was 11.0 months with a statistically significant difference in favor of the p-AML (Figure 1).
CONCLUSION
Performance status (by ECOG ≥2), age ≥60, level of leukocytes a ≥50x109/L, poor risk karyotype and s-AML subtype at diagnosis had a significant worse impact on overall survival. Most patients with s-AML came from MDS, they were older and their incidence increased as the population aged. They presented more comorbidities and worse performance status. Undoubtedly, our findings showed that s-AML is a distinct high risk subset of myeloid disorder with adverse prognosis and represents a therapeutic challenge.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal