Introduction.
MRD-tailored therapy based on pediatric-inspired intensification is a back-bone of the majority of the European study groups in adult ALL. Taking in consideration the major pitfalls of the first Russian acute lymphoblastic leukemia study group trial RALL-2009 (NCT01193933) - high CR death rate, early CNS relapses in T-ALL, selection bias in auto-HSCT vs chemotherapy comparison, absence of MRD monitoring - a new RALL-2016 protocol (NCT03462095) was introduced based on the same principles as the first one - non-intensive but non-interruptive approach with low numbers of allo-HSCT, but with further deintensification of consolidation phase, centralized MRD-monitoring and randomization for autologous HSCT with non-myeloablative conditioning (CEAM).
AIM.
To analyze the 2,5 years efficacy and to determine significance of MRD status after induction in the new Russian ongoing prospective multicenter study RALL-2016.
Materials and patients.
RALL-2016 was based on the previous RALL-2009 protocol , but one day high-dose MTX and high-dose ARA-C blocks were eliminated and substituted by 2 months of non-interruptive therapy, L-asparaginase was scheduled for 1 year of treatment instead of 2,5 y, 15 intrathecal injections were increased up to 21 mostly while consolidation phase, CR T-ALL patients were brought to randomization after the informed consent: auto-HSCT vs no auto-HSCT, - with the similar further maintenance. All primary bone samples are collected and tested for cytogenetics and molecular markers, all included patients are monitored by flow cytometry by aberrant immunophenotype in a centralized lab.
Results and discussion.
From Dec 2016 till Jul 2019 148 Ph-negative ALL pts from 10 centers were included: median age 33 y (18-54) (BCP-ALL-80 (54%) pts, T-ALL- 64 (44%), biphenotypic- 4 (2%)). CR was achieved in 84% pts. The induction death before CR was 8% (n=12), refractory ALL was registered in 12 pts (8%). Death in CR occurred in 4%.
After CR achievement 52 T-ALL patients were randomized either to chemotherapy (n=25) or to autoHSCT(n= 27). 15 of 27 T-ALL pts were transplanted at a median time of 6 months from CR (1 of 27 received alloHSCT - Neimegen Syndrom, 2 of 27 died in CR before HSCT, one pt refused the autotransplant ).
OS and DFS at 2-years constituted 70,7% and 80%. 2-y OS was 65,8% for BCP-ALL, 80% for T-ALL and 66,7% for MPAL (p=0,5). 2-y DFS was 78,7% for BCP-ALL, 83,4% for T-ALL and 100% for MPAL (p=0,88). AlloHSCT in 1st CR have received only 3 (2%) pts.
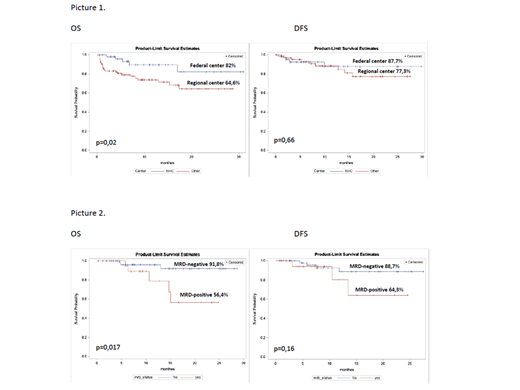
We have registered the differences in OS in pts who were treated in Federal Center (51 pts) or in Regional centers (97pts): 82% vs 64,6%, respectively (p=0,02). But there were no differences in DFS: 87,7% vs 77,3%, respectively (p=0,66) (Pic1). We have detected very high death rate in induction and in CR in the regional Centers despite the fact that the main pts characteristics were similar (median age, hyperleukocytosis, high risk group).
MRD persistence after induction (70th day of protocol) became a significant factor of poor prognosis: 2-yeasr OS and DFS in MRD-negative (59 pts) and MRD-positive (33pts) were 91,8% vs 56,4% (p=0,017) and 88,7% vs 64,3% (p=0,16), respectively (Pic 2). Median of relapse was 7 month.
Conclusion.
The new RALL-2016 study pitifully continues to demonstrate high induction and CR death rate in regional centers despite of de-intensification of chemotherapy. We've observed significant differences in OS in Federal Center vs Regionals Centers, but not in DFS.
MRD monitoring by FCM in ALL patients revealed that the persistence of MRD after induction (day+70) was an independent factor of poor prognosis and high relapse rate suggesting the introduction of new treatment approaches within a very short time after induction (maximum 3 months) in MRD positive patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal