Background
Venous thromboembolism (VTE) is a common and often fatal medical event. VTE management often includes inferior vena cava filter (IVCF) placement when anticoagulation fails or is contraindicated. Controversial indications for IVCF placement include adjunctive treatment for deep vein thrombosis (DVT) without pulmonary embolism (PE) and VTE prophylaxis for high-risk patients (Deyoung and Minocha, 2016; Ho et al., 2019). Numerous device-associated mechanical and medical complications have been described (Ayad et al., 2019) and guidelines recommend early retrieval (Morales et al., 2013). There is limited evidence, however, to guide anticoagulation practices while IVCFs are retained. We aimed to characterize IVCF placement, retrieval, and interim medical management at our institution.
Methods
Retrospective chart review was performed for all patients who underwent IVCF placement at the University of Virginia Medical Center from January to December 2016. Data were collected from time of IVCF placement until either IVCF removal or 18 months post-placement, whichever occurred first. Indication for IVCF placement, baseline patient characteristics, IVCF complications, anticoagulation regimens, and bleeding and clotting events were identified. Baseline characteristics were recorded for all patients. Patients who did not survive the admission during which the IVCF was placed, underwent IVCF removal prior to discharge, or lacked adequate outpatient records during the period of IVCF retention were excluded from the event analysis cohort.
Results
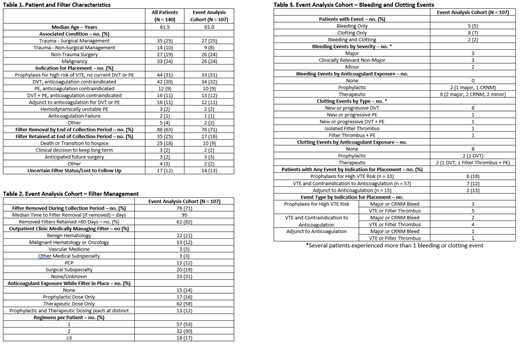
IVCFs were placed in 140 patients during the study period (Table 1). A majority of patients were admitted to a surgical service, frequently following trauma (49 patients, 35%). IVCFs were placed for several indications, most commonly diagnosed VTE with a contraindication to anticoagulation (70 patients, 50%) and prophylaxis for high risk of VTE (44 patients, 31%). By the end of the study period, 88 patients (63%) had confirmed IVCF removal while 35 patients (25%) retained the IVCF for a clinical consideration. 33 patients (24%) lacking an adequately documented period of outpatient IVCF retention were excluded from the event analysis.
Of the 107 patients included in the event analysis cohort, 76 patients (71%) underwent IVCF removal. Removal occurred >60 days after placement in 82% of these cases and median time to removal was 95 days (Table 2). Outpatient follow up and anticoagulation management varied widely, though 75 patients (70%) received a therapeutic dose anticoagulant during the period of IVCF retention and only 15 patients (14%) were not exposed to either a prophylactic or therapeutic dose anticoagulant. 50 patients (47%) had at least one regimen change.
Bleeding and/or clotting events occurred for 15 patients (14%, Table 3). All 8 bleeding events occurred during anticoagulant exposure. Patients were exposed to a therapeutic dose anticoagulant during 4 of the 6 observed major or clinically relevant non-major bleeding events. Of the 12 observed clotting events, 8 occurred in the absence of anticoagulation. Isolated DVT was the most common clotting event (8 events in 7 patients, 7%) and IVCF thrombus was observed in 2 patients (2%). Bleeding and clotting events were observed in patients with a wide range of indications for IVCF placement, including patients whose IVCFs were placed prophylactically.
Conclusions
The optimal medical management of retained IVCFs is uncertain. This retrospective study characterizes IVCF placement, removal, and interim medical management for a diverse patient population at a single institution. Outpatient follow up varied widely and anticoagulant exposure during IVCF retention was inconsistent. Despite considerable anticoagulant exposure across the cohort, major bleeding events were infrequent. Thrombotic events, often in the absence of anticoagulation and potentially preventable, were more common. Standardization of medical management during IVCF retention would likely benefit this heterogeneous patient population at high risk of both bleeding and thrombotic complications. Ongoing statistical modeling for the study cohort will seek to inform anticoagulant decision making by assessing for associations between anticoagulant exposure and these clinical events.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal