Background: Ischemic stroke is rare in young adults, with an incidence of about 10-15% of all the ischemic strokes. In about one third of these patients a cause is missing. Among patients with antiphospholipid antibodies syndrome (APS), stroke is the first thrombotic event in about 13% of cases.
Aims of our project were: to evaluate the prevalence of antiphosfolipid antibodies (aPL),to investigate on the prevalence of conventional risk factors and to define the radiological characteristics of the ischemic lesion.
Materials and methods: this is a no profit, observational multicenter prospective study. Inclusion criteria were: age older than 18 and younger than 55 years, informed written consent, a clinical and radiological diagnosis of stroke.
Patient's data were collected at diagnosis and after 30 days from stroke. If any aPL positivity was found the patient was referred to our service to further/eventually confirm the diagnosis of APS. For each patient these data were collected: age, sex, body mass index, personal and familial history, concomitant co morbidities and therapies, cardiovascular risk factors, drug abuse.
CT scan or angioCT or MRI was always performed at diagnosis, aPL profile was determined at diagnosis and eventually confirmed after 12 weeks according to the Sapporo criteria. None of the patients had a previous diagnosis of APS.
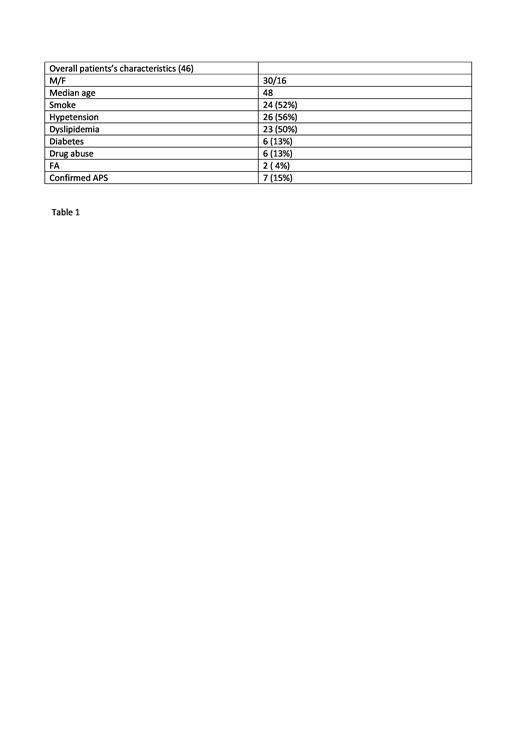
Results: enrolled patients from January 2017 to December2018 were 46 out of 425 ischemic stroke (10.8%). We found 11/46 aPL positivity patients. Among these patients, 7 were confirmed at 12 weeks (15%). Baselines characteristics of the study population are detailed in table 1. We found a high prevalence of associated conventional cardiovascular risk factors: hypertension (56%), dyslipidemia ( 50%), obesity (55%), smoke ( 52%). We didn't find any correlation between APS and a clear radiological pattern on MRI and CT scan.
Conclusions: Prevalence of APS was 15% in our cohort of young patients with stroke, 85% of which had an high risk aPL profile. The detection frequency is similar to the recent APS-ACTION and literature findings. In our cohort stroke was a relapse of a previous ischemic event in 24% of the patients, while in 15% there was a stroke's relapse. Even if these data should be confirmed with a wider number of patients, it seems to be useful to evaluate the presence of aPL in a young patient with ischemic stroke .
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal