Introduction: A serious complication in hemophilia A is the formation of inhibitors to clotting factors. The primary means for eradicating inhibitors is immune tolerance induction (ITI) therapy. Antihemophilic factor (human) (Koate®-DVI) is a purified dried concentrate indicated for the treatment of hemophilia A with insufficient activity of Factor VIII (FVIII). Although other plasma-derived concentrates containing von Willebrand factor have been utilized successfully for ITI, studies evaluating this product for ITI therapy have not been published. An evaluation of patient- and treatment-related factors associated with outcomes following primary or rescue ITI with antihemophilic factor (human) in patients with hemophilia A and inhibitors was conducted in this retrospective multicenter chart review project.
Methods: An evaluation of medical records of 13 inhibitor patients treated with antihemophilic factor (human) for primary or rescue ITI therapy between January 1, 2012, and July 31, 2017, was conducted in five US hemophilia treatment centers. To be eligible for inclusion, patients were required to have a diagnosis of hemophilia A of any severity level, inhibitor to FVIII at the time of treatment initiation with antihemophilic factor (human), and ongoing treatment with antihemophilic factor (human) for primary or rescue ITI. Data were de-identified and analyzed descriptively. Outcome measures were defined, per the International Immune Tolerance consensus recommendations, as "complete success" (inhibitor titer <0.6 Bethesda Units [BU] at 33 months of ITI, FVIII recovery ≥66% and half-life ≥6 hours), "partial success" (a reduction in inhibitor titer to <5 BU mL with FVIII recovery <66% and/or FVIII half-life <6 hours associated with clinical response to FVIII therapy not followed by a treatment-limiting anamnestic rise in inhibitors to >5 BU mL), or "failure" (neither complete nor partial success).
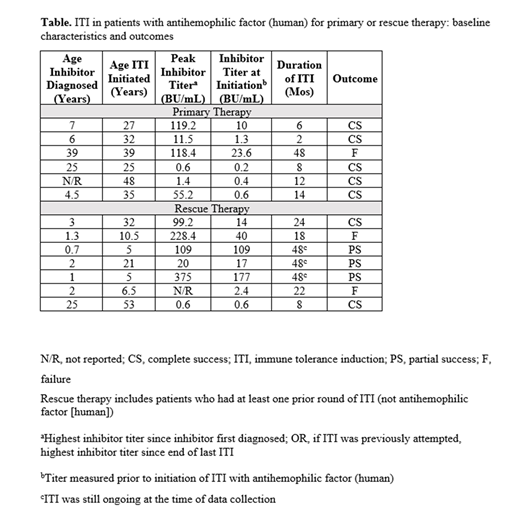
Results: All (N=13) patients who met the inclusion criteria were males with severe hemophilia, with the exception of one with moderate hemophilia. Six patients were African American, four were Hispanic, two Caucasian, and one was Asian. They were diagnosed with inhibitors between the ages of 8 months and 39 years and were 5 to 53 years old upon ITI with antihemophilic factor (human). Ten of 13 patients (76.9%) had successful ITI; seven with complete success and three with partial success (Table). Three patients failed ITI. As primary therapy, complete success was obtained with all but one of the six patients treated with antihemophilic factor (human). These six patients were all older than 7 at the initiation of ITI, a risk factor for poor ITI. Seven of the 13 total patients had a combined previous 12 attempts at ITI with other products (plasma derived and/or recombinant). Of these seven rescue patients, ITI with antihemophilic factor (human) was completely successful in two and partially successful in three. Adverse events reported once in separate patients during treatment with antihemophilic factor (human) included catheter infection, portal infection, bacteremia, peritonitis due to a ruptured appendix, and complications in treatment. One patient had several adverse events, including cellulitis at the port site, abdominal wall hematoma, right thumb fracture and hematoma, and left shoulder hemarthrosis.
Conclusions: While retrospective data has limitations, real-world evidence demonstrates that ITI with antihemophilic factor (human) concentrate can be successful or partially successful in diverse populations of moderately complex patients with hemophilia A and inhibitors. The data suggest that antihemophilic factor (human) may be most appropriate for patients when used as primary ITI, as even patients older than 7 years achieved complete success. Additional patients need to be evaluated to make a definitive conclusion regarding the impact of age on success of ITI therapy in addition to other risk factors.
Escobar:Sanofi: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees; National Hemophilia Foundation: Consultancy, Membership on an entity's Board of Directors or advisory committees; Pfizer: Consultancy, Membership on an entity's Board of Directors or advisory committees; Genentech: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novo Nordisk: Consultancy, Membership on an entity's Board of Directors or advisory committees. Rajan:Bayer, Octapharma: Consultancy, Honoraria, Research Funding, Speakers Bureau. Amega:Kedrion Biopharma: Employment.
Koate is not approved to treat vWD, nor, cTTP however, based on some published reports using kotae for these indications, we are anticipating those type of off label inquiries. I will clearly disclose to the participants that these are off label indications.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal