Introduction: Heparin induced thrombocytopenia (HIT) is a severe prothrombotic condition, usually triggered by exposure to heparin products. It is characterized by platelet activation induced by the formation of antibodies to the platelet factor 4 (PF4)/ heparin polyanion complexes. Diagnostic algorithm includes clinical scoring (4T score) alongside serological test for detection of these antibodies (HIT-Ab), while serotonin release assay (SRA) remains the gold- standard for confirmation. The automated latex immunoturbidometric assay (LIA) has recently been FDA approved as a screening tool for HIT and is a potential alternative to the conventional particle immunofiltration assay (PIFA) for time-sensitive detection of HIT-Ab to guide treatment considerations. We recently introduced LIA in our institution. In this study, we present our experience with LIA in comparison to PIFA in the diagnosis of HIT.
Methods: We retrospectively reviewed the charts of all the patients on whom a PIFA was ordered between March 2017 and March 2018 in our hospital. We collected information on the results of the PIFA and SRA (if available). We replaced PIFA with LIA for HIT screening. Then, we introduced a structured protocol for diagnosis of HIT in our institution by incorporating 4T scoring alongside LIA order in the electronic medical record (EMR), in December 2018. We reviewed the EMR of all the patients on whom HIT-Ab test (LIA) was ordered between January and June of 2019, and collected similar information as before. All the data were compiled in a single master excel sheet for calculation of performance characteristics (sensitivity, specificity, positive and negative predictive values) for both PIFA and LIA. A patient was considered to have the diagnosis of HIT if the result of SRA was available and positive.
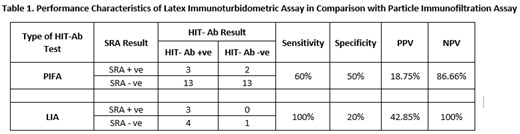
Results: In the first phase, a total of 31 orders for SRA was noted against 170 PIFA orders. Five patients had a positive SRA, of whom two were PIFA negative. Half the patients with a negative SRA result were positive for PIFA. Hence, the sensitivity and specificity of PIFA test for our study population were noted to be 60% and 50%, respectively. PIFA had a positive predictive value (PPV) of mere 18.75% for the diagnosis of HIT, whereas the negative predictive value (NPV) was found to be 86.66%. Introduction of structured protocol for HIT diagnosis substantially reduced the number of inappropriate SRA orders in the second phase. On review of data for six months with the new HIT-Ab test LIA, SRA was ordered in only eight patients, to go with 69 orders for the LIA. The result of LIA was positive in all three patients with a positive SRA, whereas it was false positive in four instances. Only one patient was negative for both LIA and SRA during this period. LIA was found to be 100% sensitive and 20% specific for the diagnosis of HIT in our sample. PPV and NPV for LIA were 42.85% and 100%, respectively.
Conclusion: The sensitivity and specificity of LIA were found to be 100% and 20%, respectively, in our study population, which is different from the earlier report (Warkentin et al. 2017). The small sample size is a limitation of our study. Higher PPV and NPV for LIA, with its quick turnaround time, make it a useful alternative for the time-sensitive determination of post-test probability for HIT in patients.
[HIT- Ab- Heparin Induced Thrombocytopenia Antibody, PIFA- Particle Immunofiltration Assay, LIA- Latex Immunoturbidometric Assay, SRA- Serotonin Release Assay, +ve- Positive, -ve - Negative, PPV- Positive Predictive Value, NPV- Negative Predictive Value]
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal