Introduction
Herpes zoster (HZ) after hematopoietic cell transplant (HCT) is a well-known complication with a peak incidence during the first year post-HCT. Cord blood transplant (CBT) recipients are at increased risk for viral infections and historically have a cumulative incidence of HZ approaching 80% by 2.5 years in the context of short-term peri-HCT antiviral prophylaxis. In 2009, international guidelines for prevention of infections after HCT recommended maintaining HZ prophylaxis for at least 1 year after HCT. We retrospectively studied the impact of longer-term antiviral prophylaxis on the incidence of HZ after CBT.
Methods
Between 2006 and 2016, we performed 360 CBT at our Institution. Patients who were seronegative for varicella zoster virus (VZV) or received the live varicella vaccine (i.e. Varivax®) pre-CBT without a history of chickenpox or HZ were excluded. From 2006-2008, CBT recipients received acyclovir (ACV) 800 mg BID or valacyclovir (VACV) 500 mg BID for HSV and VZV prophylaxis. From 2008-2016, patients who were CMV seropositive received higher-dose prophylaxis with VACV 2g TID through day +100. Before 2009, institutional guidelines recommended to continue prophylaxis until the end of immunosuppression; after 2009, prophylaxis was recommended for at least 1 year and until 8 months after immunosuppression ends. For patients discharged from our center, data were collected through standardized questionnaires and medical records. We abstracted HZ events and other variables for up to 5 years post-CBT. We calculated the cumulative incidence of HZ after CBT, treating death and second HCT as competing risk events. Variables were evaluated for an association with development of HZ using Cox proportional hazards regression; those of biological interest and with a P value ≤ 0.3 in univariable analyses were considerate for multivariable model.
Results
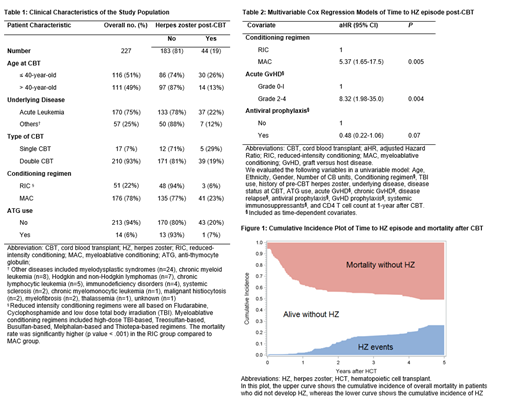
The study cohort consisted of 227 CBT recipients with a median follow up of 25.4 months (interquartile range [IQR], 6.8 - 49). Follow up time was truncated at the time of death (n=113), second HCT (n=13) or last available records (n=32). Cohort characteristics are shown in Table 1. Among 1-year survivors, 91% were still receiving prophylaxis for a median duration of 20.6 months post-CBT (IQR, 14.1 - 29.4). HZ occurred in 44 patients (19%) at a median of 23.6 months (IQR, 16.1 - 30.3). Most patients (n=31/44, 70%) were not taking antiviral prophylaxis when HZ developed. The cumulative incidence of HZ by 1-year post-CBT was low (1.8%; 95% CI, 0.1%-4%) but increased starting from the second year and reached 26% (95% CI, 19%-33%) by 5 years (Figure 1). Disseminated HZ occurred in 5 cases (11%), and post-herpetic neuralgia occurred in 14 cases (31.8%). Of the 13 HZ episodes that occurred in patients reportedly taking antiviral prophylaxis, 6/13 had clear documentation of ongoing antiviral prophylaxis and 5/13 were still receiving immunosuppressive treatment for graft-versus-host disease (GvHD). All patients responded to antiviral treatment, which consisted of ACV (n=18), VACV (n=16), and famciclovir (n=1).
In a multivariable analysis, patients who received myeloablative conditioning or had acute GvHD grades 2-4 had a higher risk of HZ, whereas the use of antiviral prophylaxis was associated with a lower risk of HZ (Table 2). Among 35 patients who discontinued prophylaxis before completing immunosuppressive therapy, 28.5% developed HZ. We found no association between CD4+ T cell counts at 1-year after-CBT and HZ risk.
Conclusions
In this cohort of 227 CBT recipients with up to 5 years of follow up, the cumulative incidence of HZ was 26% at 5 years, despite antiviral prophylaxis for >1 year in the majority of patients. Furthermore, these patients had high rates of post-herpetic neuralgia and disseminated VZV. Antiviral prophylaxis protected against HZ but there were breakthrough cases. Given that a high number of patients interrupted prophylaxis while still receiving immunosuppressants, adherence to antiviral prophylaxis should be emphasized by health care providers. Based on our findings, the lack of alternative prophylactic strategies at this time, and the safety of ACV/VACV, longer duration of prophylaxis should be considered, especially in patients with ongoing immunosuppression. Recent data demonstrating the safety and efficacy of the HZ subunit vaccine after autologous HCT support future study of HZ vaccination after allogeneic HCT.
Delaney:Nohla Therapeutics: Employment, Equity Ownership; Biolife Solutions: Membership on an entity's Board of Directors or advisory committees. Boeckh:Chimerix: Research Funding; GSK: Other: Personal fees; GSK: Research Funding; Merck: Research Funding; Merck: Other: Personal fees; Clinigen: Other: Personal fees. Milano:ExCellThera: Research Funding; Amgen: Research Funding. Hill:Takeda: Other: research support; Karius: Other: research support; Amplyx: Consultancy; Nohla Therapeutics: Consultancy, Other: research support.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal