Introduction: Graft failure (GF) and poor graft function (PGF) are severe complications after allogeneic hematopoietic cell transplantation (alloHCT) that can result in substantial morbidity and mortality. Haploidentical hematopoietic cell transplantation (haploHCT) has historically been associated with high graft failure rates, particularly after RIC conditioning, largely due to the intense bi-directional alloreactive reactions between donor and recipient. To overcome this, a strategy using a T-cell replete graft with posttransplant cyclophosphamide (PTCy) was developed and significantly improved engraftment. Despite the promising outcomes of haploHCT with PTCy, graft failure rates are still reportedly higher than regimens used in the non-haploidentical transplant setting. To assess incidence and possible risk factors for GF/PGF in these patients, we retrospectively analyzed data from a single transplant center.
Methods: We performed a retrospective study of all patients who underwent first RIC haploHCT using PTCy and RIC 8/8 MRD HCT at Dana-Farber Cancer Institute from January 2012 to June 2018. The primary objective was the incidence of GF/PGF. Secondary objectives included (1) predisposing risk factors for GF/PGF, (2) the need and efficacy for CD34+ selected stem cell boost and/or second transplant for GF/PGF and (3) the impact of GF/PGF on survival outcome. Primary GF was defined as (1) absence of disease relapse AND (2) never having reached an ANC 500 x109/L for 3 consecutive days within 50 days post-transplant OR (3) having reached an ANC >500 x109/L for 3 consecutive days but having low or falling total chimerism (<25%) within 30 days post-transplant. Secondary GF was defined as (1) having lost a graft (<25% donor chimerism) after sustained initial engraftment with total donor chimerism >70%, occurring >100 days post-transplant + 2 lines of cytopenias. PGF was defined as poor cell counts (at least 2 lines of cytopenias) occurring > 50 days post-transplant despite evidence of donor engraftment with a total peripheral donor chimerism >70%. Incidence of GF/PGF was calculated in a competing risk framework.
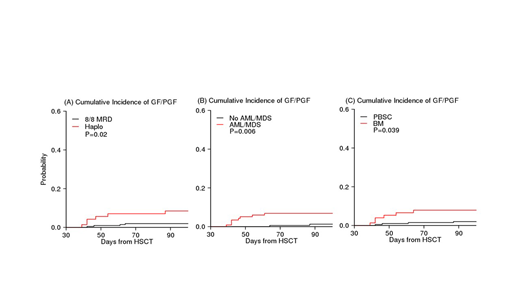
Results: A total of 278 (haplo, N=71; 8/8 MRD, N=207) patients met eligibility criteria. 76% in the haploHCT and 11% in the MRD cohort received bone marrow as graft source (p<0.0001). The 100-day cumulative incidence of GF/PGF was significantly higher in the haploHCT compared to the MRD cohort 8.5% (95% CI, 3.4% to 16%) vs 2% (95%CI, 0.6% to 4.6%), respectively, (p=0.023), Figure A. The majority (>=80%) of GF/PGF in both cohorts was due to poor graft function. While most patients had initial engraftment, time to engraftment was significantly longer in haploHCT recipients compared to the MRD cohort: median time to ANC >500 x109/L, 17 vs. 14 days, (p<0.01); median time to platelets <20,000 x109/L, 26 vs. 18 days, (p<0.01). In addition to haploHCT, a preceding diagnosis of AML/MDS (P=0.006) and bone marrow graft (P=0.039) were risk factors for GF/PGF, Figures B-C. For patients with GF/PGF in the haploHCT cohort, 3 (50%) received a CD34+ selected stem cell boost and 3 (50%) received a second transplant. There was no difference in outcomes between these two treatments. In the MRD cohort, 3 (60%) received a CD34 selected stem cell boost, 1 (20%) immunosuppressive reduction only and 1 (20%) no treatment. In multivariable analysis treating GF/PGF as a time dependent variable, the hazard ratio (HR) of GF/PGF was 11.0 (95% CI 3.1-39), P=0.0002 for NRM. When an interaction between GF/PGF and cohort was tested, the HR of GF/PGF was significantly worse in the haploHCT cohort compared to the MRD cohort (HR 20 vs 5, respectively). Indeed, 4 out of 6 GF/PGF died within 6 months of GF/PGF in the haploHCT compared to only one died within 6 months in the MRD cohort. The HR of GF/PGF was 1.8 (P=0.19) for OS and 1.93 (P=0.11) for PFS.
Conclusion: In this single center retrospective analysis of 278 patients, the incidence of GF/PGF was significantly higher in haploHCT recipients compared to 8/8 MRD recipients. GF/PGF was associated with an increased risk of NRM, particularly in the haploHCT cohort. We also identified other predisposing risk factors for GF/PGF, including a preceding diagnosis of AML/MDS and the well-established risk factor of bone marrow graft source. Both CD34+ selected stem cell boost and second transplant are reasonable rescue therapies in the haploHCT and survival was similar after these two rescue therapies.
Nikiforow:Kite/Gilead: Honoraria; Novartis: Honoraria; NKarta: Honoraria. Koreth:Equillium: Consultancy; Amgen: Consultancy; Cugene: Consultancy. Ritz:TScan Therapeutics: Consultancy; Talaris Therapeutics: Consultancy; Draper Labs: Consultancy; LifeVault Bio: Consultancy; Avrobio: Consultancy; Celgene: Consultancy; Aleta Biotherapeutics: Consultancy; Merck: Research Funding; Kite Pharma: Research Funding; Equillium: Research Funding. Ho:Jazz Pharmaceuticals: Consultancy; Jazz Pharmaceuticals: Research Funding; Omeros Corporation: Membership on an entity's Board of Directors or advisory committees. Soiffer:Cugene: Consultancy; Mana therapeutic: Consultancy; Jazz: Consultancy; Gilead, Mana therapeutic, Cugene, Jazz: Consultancy; Kiadis: Other: supervisory board; Juno, kiadis: Membership on an entity's Board of Directors or advisory committees, Other: DSMB. Cutler:Incyte: Consultancy; Jazz: Consultancy; Pharmacyclics: Consultancy; Fate Therapeutics: Consultancy; Genentech: Consultancy; BMS: Consultancy; ElsaLys: Consultancy; Kalytera: Other: DSMB; Cellect: Other: DSMB; BiolineRx: Other: DSMB; Kadmon: Consultancy; Omeros: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal