Background: Myelodysplastic syndrome (MDS) therapeutic decisions have been traditionally based on the International Prognostic Scoring System (IPSS) (Greenberg et al, Blood 1997) and IPSS-R (Greenberg et al, Blood 2012). Recently, next-generation sequencing genetics has been incorporated into management of MDS, however its use is limited in routine clinical practice. Current prognostic models do not allow the identification of patients with low risk disease (low or intermediate-1 IPSS) and poor prognosis, who could benefit from an early intervention. Garcia-Manero et al (Leukemia 2008) described a specific prognostic scoring system for this subgroup of patients (LR-PSS) based on age ≥60 years, hemoglobin <10g/dl, platelet count <50k/uL or 50-200k/uL, bone marrow blasts ≥4% and unfavorable cytogenetics (non-del(5q), non-diploid). This LR-PSS score system enables the stratification of low risk MDS patients into 3 different risk categories; interestingly, the third category identifies a subgroup of patients with a median overall survival (OS) similar to that of patients classified as intermediate-2 and high risk IPSS. Besides, the IPSS-R described by Greenberg et al (Blood 2012) has demonstrated a strong prognostic value for OS and LFS as compared to the IPSS when applied to different independent series of MDS patients. The prognostic impact of the LR-PSS has not been analyzed in MDS patients with very low-, low- and intermediate IPSS-R scores.
Aim: To analyze the prognostic value of Low Risk Prognostic Scoring System(LR-PSS) in a population of lower risk MDS patients (very low, low and intermediate IPSS-R) analyzing as endpoints overall survival (OS) and leukemia free survival (LFS).
Methods: A total of 890 consecutive patients with MDS (01/1992-7/2018) diagnosed at the Catalan Institute of Oncology in Barcelona were included in the study. 539 (60%) had available cytogenetics and therefore, IPSS-R could be assessed. 474 (88%) patients were classified as very low, low and intermediate IPSS-R and were included in the study.
Results: 178 (37.6%) patients were classified as very low, 219 (46.2%) low and 77 (16.2%) intermediated IPSS-R risk MDS. Median age at diagnosis was 73 years (range 32-101). 332 (70%) were male. According to the 2008 WHO classification, 2.5% CRDU, 7.4% RA, 42.2% RCMD, 13.7% RAEB‐1, 3.6% RAEB‐2, 26.4% CMML and 4.2% MDS‐U with isolated 5q deletion. At diagnosis, median hemoglobin, platelet and bone marrow blast were 11.6 g/dL (5.5-17.1), 157 x109/L (1-1492) and 2 % (0-17), respectively. 84 (17.7%) patients had unfavorable LR-PSS cytogenetics at diagnosis. Median follow up time for survivors was 5.4 years (range 0.25-23.8). At the time of last follow up, 58.4 % (277) had died and 71 (15%) had progressed to acute myeloid leukemia.
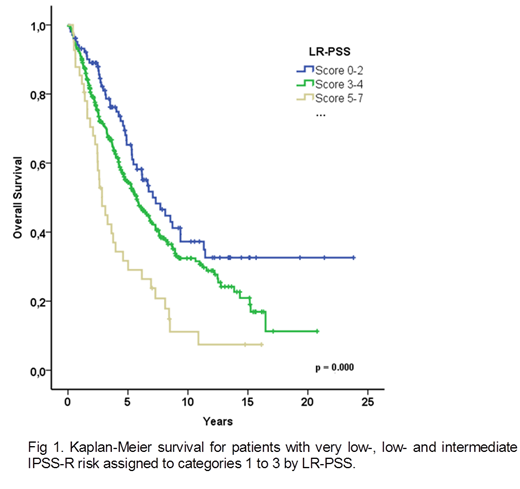
When the LR-PSS was applied to the very low, low and intermediate IPSS-R subgroups, three well-differentiated prognostic categories could be identified: 103 patients (21.7%) category 1 (scores 0-2); 330 (69.6%) patients category 2 (scores 3-4) and 41 (8.7%) patients category 3 (scores 5-7) with significant different OS and LFS. Median OS for categories 1, 2 and were 7.1 years (95% CI 4.9-9.2), 5.7 years (95% CI 4.7-6.7) and 2.8 years (95% CI 2.1-3.6), p<0.001 (Figure 1), respectively. Rate of progression to acute myeloid leukemia was 10% (10/99), 15% (48/323) and 27% (11/411) for categories 1, 2 and 3, respectively.
Summary/Conclusion: When applied to a low risk (very low, low and intermediate) IPSS-R cohort of MDS population, LR-PSS identifies a subgroup of patients with a significantly worse prognosis who could benefit from an early treatment intervention.
Sureda:Janssen: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Gilead: Consultancy; Roche: Honoraria; BMS: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria; Takeda: Consultancy, Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal