Background
With lymphoma survival rates increasing and a growing population of long-term survivors, the development of cardiovascular disease (CVD) in this patient population is of increasing importance. Anthracyclines are critical in the management of many lymphoma subtypes. However, there is a risk of developing anthracycline-induced CVD. Here, we estimate the cumulative incidence of CVD in adult lymphoma survivors and investigate risk factors associated with post diagnosis CVD.
Methods
Participants were from the Mayo component of the Molecular Epidemiology Resource (MER) of the University of Iowa/Mayo Clinic Lymphoma Specialized Program of Research Excellence (SPORE). From 2002-2015, the MER offered enrollment to all patients with newly diagnosed lymphoma who are US residents and age >18 years. Participants completed a risk factor questionnaire, and clinical and treatment data were abstracted from medical records. Patients were contacted every 6 months for the first 3 years after diagnosis and annually thereafter to assess disease status, re-treatment and new onset morbidity including CVD. CVD events, including congestive heart failure (CHF), coronary artery disease (CAD), valvular heart disease (VHD), and arrhythmia were identified and validated against medical records. CHF was validated with the Cardiovascular Health Study Criteria and/or the Framingham Criteria. CAD, arrhythmia, and VHD were validated using clinical definitions. We calculated the cumulative incidence of CVD, with death modeled as a competing risk. The association of risk factors and treatments with risk of CVD was estimated using hazard ratios (HR) and 95% confidence intervals (CI) from Cox regression with a competing risk of death. Risk factors included age, sex, diabetes, smoking, body mass index (BMI), and treatment with anthracyclines or radiation therapy.
Results
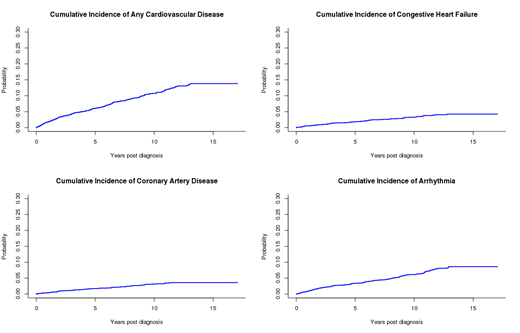
The study consisted of 3,063 lymphoma patients after excluding those with chronic lymphocytic leukemia and CVD prior to lymphoma diagnosis. The median age at diagnosis was 59 years (range 18-95), and 56% were males. At a median follow-up was 6.9 years (range 0.8-17.1), 640 patients (21%) had died without CVD and 485 patients self-reported CVD post lymphoma diagnosis, of which 280 (57.7%) were validated. Cardiovascular events included 86 CHF, 78 CAD, 40 VHD, and 164 arrhythmias. The cumulative incidence of CVD (Figure 1) at 5 and 10 years was 6.0% (95% 5.2%-7.0%) and 10.7% (95% CI 9.5%-12.1%), respectively. In multivariable analysis, increasing age (HR=3.93 per 5 years, p<0.001), male sex (HR=1.33, p=0.03), former smoker (HR=1.04, p=0.77), current smoker (HR=1.96, p<0.001), BMI>30 kg/m2 (HR=1.50, p=0.01), and anthracycline treatment (HR=1.49. p<0.001) were all significantly associated with risk of overall CVD, while there was no association with diabetes (HR=0.92, p=0.70) or radiation therapy (HR=1.05, p=0.78) in the multivariable model. Anthracycline use was significantly associated with increased risk of CHF (HR=2.64, p<0.001) and arrhythmia (HR=1.51, p<0.01), but not VHD (HR=0.83, p=0.56) or CAD (HR=1.23, p=0.31) after adjustment for the cardiac risk factors. The number of anthracycline cycles ranged from 0 to 12. 63.2% of individuals that received anthracyclines received 6 cycles. The 5-year cumulative incidence of CVD for 0, 1-5, 6, and >6 anthracycline cycles was 5%, 6.9%, 7.4%, and 7.7%, respectively. Adjusting for cardiac risk factors, the number of anthracycline cycles was significantly associated with increased risk of CVD (1-5 cycles HR=1.34, p=0.11; 6 cycles HR=1.51, p<0.01; >6 cycles HR=2.04, p=0.03). Furthermore, the number of anthracycline cycles was associated with CHF (1-5 cycles HR=2.82, p<0.001; 6 cycles HR=2.46, p<0.001; >6 cycles HR=5.33, p<0.001) and arrhythmia (1-5 cycles HR=1.31, p=0.27; 6 cycles HR=1.60, p<0.01; >6 cycles HR=1.65, p=0.27).
Conclusions
In the modern treatment era, the risk of new onset CVD in patients with lymphoma without a history of CVD is approximately 1% per year after diagnosis. Arrhythmia and CHF were the most commonly occurring CVD events in this cohort. Both traditional CVD risk factors and treatment with anthracyclines was associated with an increased risk of developing CVD, and anthracyclines were a risk factor for arrhythmia and CHF in particular. Prevention of CVD in lymphoma patients will need to address both treatment and traditional lifestyle factors.
Maurer:Morphosys: Membership on an entity's Board of Directors or advisory committees; Nanostring: Research Funding; Celgene: Research Funding. Nowakowski:Selvita: Membership on an entity's Board of Directors or advisory committees; Genentech, Inc.: Research Funding; F. Hoffmann-La Roche Ltd: Research Funding; Curis: Research Funding; Bayer: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; NanoString: Research Funding; MorphoSys: Consultancy, Research Funding. Cerhan:NanoString: Research Funding; Celgene: Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal