Background: Numerous studies have demonstrated superior survival for adolescents and young adults (AYA) with acute lymphoblastic leukemia (ALL) treated with pediatric-inspired as opposed to adult-type front-line ALL regimens. However, very little is known regarding the potential impact of therapeutic regimen type on late effects and subsequent neoplasms (SN) in AYA ALL survivors. Using population-based data, we describe associations between subsequent medical conditions/SN, sociodemographics, and ALL therapies, including regimen type (pediatric versus adult) in a large cohort of AYA ALL survivors.
Methods: The California Cancer Registry (CCR) linked with California hospitalization data was used to evaluate socio-demographics, therapies, and subsequent medical conditions (late effects) amongst AYAs (15-39 years) diagnosed with ALL in California between 1995-2012 surviving a minimum of three years from diagnosis. The CCR was used to identify front-line therapeutic regimen, receipt of cranial irradiation (CRI), and SN; hematopoietic cell transplantation (HCT) and late effects were captured through hospitalization data. Late effects were categorized as cardiac (hypertensive disease, coronary artery disease, heart failure), neurologic (stroke, seizure), endocrine (thyroid disease, diabetes, ovarian/testicular dysfunction, other metabolic diseases), respiratory (asthma, chronic obstructive pulmonary disease, pulmonary fibrosis), renal (chronic kidney disease, hemodialysis, kidney transplant), liver (chronic liver disease, pancreatitis, cirrhosis, liver transplant), and avascular necrosis (AVN). The 10-year cumulative incidence (CMI) of developing each late effect/SN was estimated, accounting for death as a competing risk. Multivariable Cox proportional hazards regression analyses (MVA) examined the impact of sociodemographic factors and therapies (pediatric vs adult ALL regimen, HCT, CRI) on the occurrence of each late effect/SN. Front-line regimen type (pediatric vs adult) was highly correlated with receipt of HCT (P<0.001); thus, the impact of front-line regimen was evaluated in separate MVA for those who did and did not receive HCT.
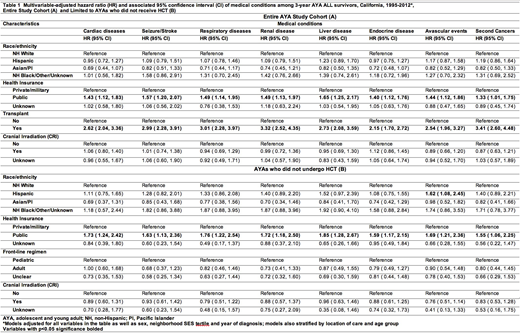
Results: Of the 1,069 survivors of AYA ALL (median follow-up, 8.2 years), 44% were 15-19 years at diagnosis, 32% were 20-29 years, 24% were 30-39 years; 62% were male and 50% were Hispanic. Thirty-nine percent resided in the lowest neighborhood socio-economic status (SES) tertile and 35% had public or no insurance. The majority (60%) received an adult-type front-line ALL regimen; 19% received CRI and 28% underwent HCT. Twenty-four SN occurred; thyroid, head and neck, and breast cancers were most common. The 10-year CMI of endocrine disease (29%) and cardiac disease (17%) were strikingly high; AVN (10%), respiratory disease (6%), liver disease (7%), seizure/stroke (4%), renal disease (3%) and SN (3%) occurred with descending incidence. Multivariable analyses including the entire patient cohort demonstrated that public or no insurance (vs private/military insurance) and receipt of HCT were independently associated with both late effects across organ systems and SN (Table 1A). Race/ethnicity, sex and neighborhood SES were not associated with late effects/SN. In MVA limited to the 766 AYAs who did not receive HCT, we continued to find a significant association between public and no insurance and all late effects, including SN. Front-line regimen type was not significantly associated with any of the late effect categories, nor was CRI (Table 1B). Among the 303 AYAs who received HCT, lower neighborhood SES was associated with higher risk of all late effects/SN considered.
Conclusions: This large population-based analysis is amongst the first to describe late effects and SN in survivors of AYA ALL. Public or no health insurance and receipt of HCT were independently associated with the development of late effects across organ systems and SN, while front-line regimen type (adult vs. pediatric) among non-transplanted AYAs was not. The strong association between insurance type and late effects suggests that AYAs with public or no insurance may have reduced access to survivorship care following completion of ALL therapy. While additional follow-up is necessary to discern the full burden of late effects in survivors of AYA ALL, these findings suggest significant ongoing healthcare needs in this cancer survivor population.
Muffly:KITE: Consultancy; Pfizer: Consultancy; Adaptive: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal