Background:
Vincristine- or vinblastine-induced peripheral neuropathy (VIPN) is a common adverse event during lymphoma treatment that can profoundly impact quality of life and survivorship. VIPN often leads to dose-reduction or discontinuation of these agents. However, there is limited data (Annals of Hematology, Utsu 2016; Annals of Hematology, Morth 2018) evaluating the impact of dose reduction or omission of vinca alkaloids on progression-free survival (PFS) or overall survival (OS). We report on a series of lymphoma patients (pts) who had vincristine (Vn) or vinblastine (Vb) dose-reduced or omitted from their initial chemotherapy.
Methods:
We performed a retrospective chart review of lymphoma pts who were seen in consultation at the University of Colorado from 2015 to 2018. Data included demographics, lymphoma subtypes, Vn- or Vb-containing treatment regimens, PFS, and OS. PFS and OS were examined using Kaplan-Meier method, and stratification techniques were used to compare survival based on full dose versus dose-reduced/omitted treatments. Cox regression methods were used to assess the impact of refractory or progressive disease, disease stage, and prognostic score on PFS.
Results:
373 pts who received Vn- or Vb-containing chemotherapy were identified. Of those, 228 pts had complete records available for review for treatment, response and survival data. 133 pts (58.3%) were male. Median age was 56 years (range 19 to 85 years). The most common diagnoses were diffuse large B-cell (59.2%), Hodgkin (26.3%), follicular (8.3%), PTLD (3.1%), Burkitt, (2.6%), and gray zone (0.4%) lymphomas. Chemotherapy regimens administered were REPOCH (35.1%), RCHOP (32.9%), and ABVD/AVD (21.9%). Incidence of neuropathy during treatment was 36.4%. The median follow up is 23.7 months (range 2.5 to 150.7 months). We categorized patients into 2 groups based on chemotherapy dosing: full dose (Group 1: n=155/228; 68%) and dose-reduced or omitted (Group 2: n= 73/228; 32%). There was not a significant difference in stage or prognostic score between Group 1 and Group 2.
Group 2 was further sub-categorized into Subgroup 2A (patients with Vn/Vb omitted at any point: n= 46/228; 20.2%) and Subgroup 2B (patients with Vn/Vb dose-reduced: n=27/228; 11.8% ). Of the 73 patients in Group 2, 67 patients had Vn/Vb omitted or reduced due to neuropathy; 6 patients had the drugs omitted (5/73) or reduced (1/73) due to GI side effects.
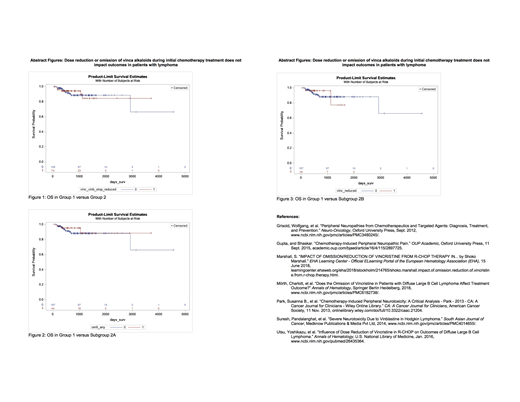
Complete response (CR) rates between Group 1 and Group 2 were similar (81.3% vs 87.7%, respectively). Patients in Group 1 had a higher number of patients with relapsed/refractory disease compared to Group 2 (p<0.01). PFS was better in Group 2 compared to Group 1 (p=0.027). There was no significant difference in OS between the two groups (p=0.83) (Figure 1).
There was no significant difference in response rates, PFS, or OS when comparing Subgroup 2A to Group 1 and Subgroup 2B to Group 1 (Figures 2 and 3). There was also no statistically significant difference in response rate, PFS, or OS if Vn/Vb was dose reduced early (first half of total cycles) versus late, when comparing Group 1 versus Group 2, Subgroup 2A, or Subgroup 2B.
Conclusions:
Our single-center retrospective analysis of patients suggests that reduction or omission of vinca alkaloids from initial chemotherapy does not deleteriously affect outcomes in lymphoma pts. Prospective clinical trials are underway investigating the substitution of vinca alkaloids with novel targeted agents. Our findings further validate the rationale and design of these contemporary trials.
Kamdar:University of Colorado: Employment; Celgene: Consultancy; Pharmacyclics: Consultancy; AstraZeneca: Consultancy; Seattle Genetics: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal