Backgrounds and Purposes
Minimal residual disease (MRD) monitoring has been proved to be the most important prognostic predictor in childhood acute lymphoblastic leukemia (ALL). The nationwide TPOG-ALL-2013 protocol (TPOG-2013), adapted from the St. Jude Total Therapy XV Study and Total Therapy XVI Study, was launched since January 2013. This is the first MRD-directed protocol for treatment of childhood ALL in Taiwan. Here, we report the improved treatment outcomes and the impacts of adherence to MRD time points.
Patients and Methods
Totally, 402 patients aged between 1-18 years and diagnosed before December 31, 2018, who had MRD monitoring at the major central laboratory (Chang Gung Memorial Hospital-Linkou), were enrolled with the last follow-up on June 30, 2019. According to TPOG-2013, two MRD measurements were scheduled on days 15-19 of induction (MRD1 time point, TP1) and days 35-42, end of induction (MRD2 time point, TP2) to make the definitive risk stratification to guide subsequent therapy.
The methodologies of MRD measurement included multicolor flow cytometry for leukemia-associated immunophenotypes (LAIP) (82.3% of TPOG-2013 cohort), qPCR assay for clonally rearranged antigen-receptor genes (Ig/TCR) if no LAIP (12.5%). Since January 2018, reverse transcription real-time quantitative polymerase chain reaction (RT-qPCR) was applied to patients carrying fusion transcripts (5.2%) of TCF3-PBX1, ETV6-RUNX1, BCR-ABL1, KMT2A-AFF1 (AF4) and KMT2A-MLLT3. The clinical features and outcomes of patients treated with TPOG-2013 were compared with those of 1,300 patients treated with the previous TPOG-ALL-2002 protocol (TPOG-2002), which did not integrate the MRD monitoring.
Results
The median follow-up time of the 402 patients of TPOG-2013 cohort was 32.5 months (range, 1.0-79.2 months). There were no significant differences in gender, age, WBC counts, and lineage at diagnosis between the patients treated with TPOG-2002 and TPOG-2013. However, based on the MRD data, the percentages of patients assigned to each risk group of TPOG-2013 was statistically differed from those of TPOG-2002 (P< 0.0001). The 5-year event-free survival (EFS) (% ± SE) was significantly improved from 78.1 ± 1.2 of TPOG-2002 to 85.4 ± 2.5 of TPOG-2013 (P< 0.0001). Further, the cumulative incidences (% ± SE) of isolated CNS relapse and any CNS relapse significantly decreased from 4.0 ± 0.5 to 0.3 ± 0.3 (P= 0.001) and from 5.8 ± 0.7 to 1.2 ± 0.9 (P= 0.001), respectively.
The issue of non-adherence to MRD monitoring emerged since the implementation of MRD-directed TPOG-2013. For further analysis, 321 (80%) patients with exact adherence (EA) to both TPs were assigned as MRD EA group; 80 (20%) patients who were non-adherence (NA) to either one of TPs as MRD NA group; and one patient died between the two TPs was excluded for the comparative outcome analysis. The rate of non-adherence decreased significantly from 26.5% in 2013 to 2.4% in 2018. The major causes of non-adherence for both TPs were delaying MRD monitoring due to neutropenic fever and documented infections. In MRD EA group, 12.5% of patients were upgraded to higher-risk treatment groups based on their MRD results. The MRD NA group had older age (≥ 10 years), lower standard-risk and lower incidence of ETV6-RUNX1 compared with MRD EA group.
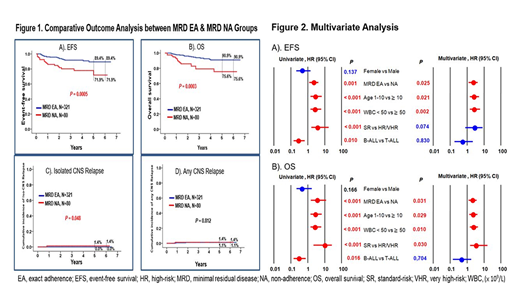
There were significant differences in outcomes between MRD EA and MRD NA groups: the 5-year EFS were 89.4 ± 2.4 and 71.9 ± 7.4, respectively (P= 0.0005), overall survival (OS) were 90.9 ± 2.1 and 75.6 ± 5.8, respectively (P= 0.0003), and the cumulative incidence of isolated CNS relapse were 0 and 1.4 ± 1.3, respectively (P= 0.048) (Figure 1). In multivariate analysis, older age (≥ 10 years), higher WBC count (≥ 50 × 109/L) at diagnosis and MRD non-adherence were independent predictors for inferior EFS. In addition to these three factors, a higher-risk classification also predicted an inferior OS (Figure 2).
Conclusions
Contemporary MRD-directed therapy has improved the treatment outcomes of childhood ALL in Taiwan. The adherence to MRD time points remains a significantly prognostic predictor in the era of MRD-guided treatment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal