Purpose
Equilibrium between red blood cells (RBC) production and clearance maintains an appropriate circulating RBC biomass. During anemia or hypoxia, a well-characterized hypoxia-dependent induction of erythropoietin (EPO) synthesis leads to an increase in RBC production. At the other extremity of the RBC lifespan, age-related modifications of RBC properties are expected to be recognized by the mononuclear phagocytic system (MPS) and trigger their clearance. We reasoned that, like RBC production, RBC clearance might be physiologically regulated by hypoxia and therefore that its downregulation could contribute to maintain an appropriate RBC biomass. A mouse model was used to explore specific hypotheses on potential regulatory mechanisms involved in RBC clearance.
Material and methods
Two steps in vivo biotinylation was used to evaluate the impact of EPO on 3 RBC subpopulations: a young subpopulation (<25 days at treatment initiation) representing the RBC produced, one of intermediate age (25-34 days at treatment initiation) which is neither produced nor eliminated, and an old one (> 34 days at treatment initiation) that is steadily cleared. A model of RBC banking (leucocyte depleted and stored in CPDA solution) was used to evaluate the clearance after transfusion of fluorescently-labeled storage-damaged RBC by flow cytometry. Different recipient models were used to evaluate the impact of specific parameters on RBC clearance including: phlebotomy-induced anemia, normobaric hypoxia, erythropoiesis-stimulating agent (ESA) treatment (darbepoietin), splenectomy, doxorubicin-induced inhibition of erythropoiesis and EPO neutralization (anti-EPO rabbit serum) either alone or in combination.
Results
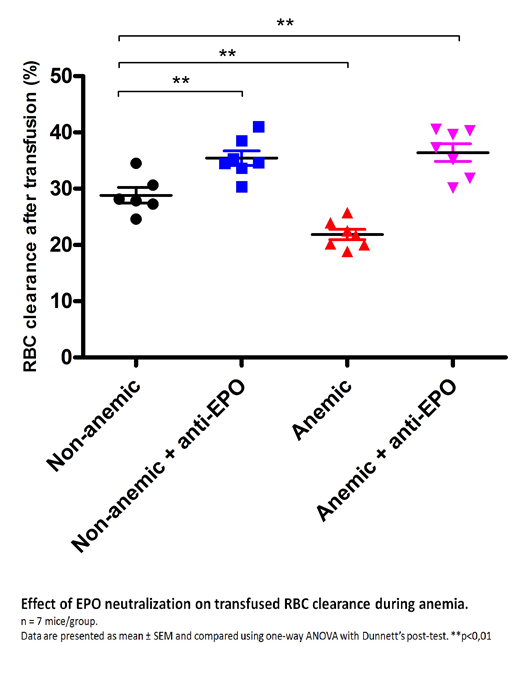
Decreased clearance of the oldest subpopulation was observed 2 days after ESA treatment and before the increase in RBC production (7 days). After 20 days of treatment, an increased number of RBC from the oldest subpopulation was detected in circulation confirming that senescent RBC clearance is sensitive to EPO signaling. After transfusion, clearance of storage-damaged RBC is reduced by 30% in anemic recipients when compared to non-anemic recipients. RBC clearance is significantly reduced in hypoxic non-anemic recipients, as soon as 6 hours after the initiation of hypoxia, suggesting that hematocrit per se does not affect RBC clearance. In ESA-treated non-anemic non-hypoxic mice, RBC clearance is also reduced showing that EPO signaling is sufficient. To investigate the role of the spleen in this process, splenectomy was combined with the previous models. As expected, RBC clearance was reduced by 20% in splenectomized recipients. RBC clearance is however even more decreased when splenectomy is combined with anemia, hypoxia or ESA treatment compared to splenectomized or control mice, suggesting that EPO downregulation of RBC clearance is not restricted to the spleen. Erythropoiesis inhibition did not alter the anemia-induced downregulation of RBC clearance ruling out the possibility that an erythroid factor is involved in the process. Finally, neutralization of circulating EPO not only abolishes the reduction of RBC clearance observed in anemic recipients, but also increases RBC clearance in both anemic and non-anemic recipients. Taken together these results indicate that EPO regulates RBC clearance during anemia and in steady state (Figure).
Conclusion
RBC clearance is downregulated during anemia/hypoxia and EPO is sufficient and necessary to mediate this physiological function. RBC clearance downregulation preceded the increase in production rate induced by ESA treatment suggesting it is a very early physiological response to maintain oxygen supply during anemia. The lifespan of a circulating RBC is therefore adaptable and could be regulated by 2 factors: the RBC pro- and anti-phagocytic properties on one side and, on the other side, the MPS level of activity and sensitivity toward these RBC properties. In case of anemia or hypoxia, increased EPO level would act on the RBC itself, on the activity/sensitivity of the MPS or both to downregulate RBC clearance until the equilibrium between oxygen need and supply is restored. Future studies will evaluate if the pathological dysregulation of this mechanism participates in the pathogenesis of anemia or, modulate transfusion efficacy and burden in chronically transfused patients.
Buffet:Zimmer Biomet: Research Funding. Hermine:Celgene: Research Funding; Novartis: Research Funding; AB science: Consultancy, Equity Ownership, Honoraria, Research Funding. Amireault:Zimmer Biomet: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal