Background: Patients with cancer are at elevated risk for venous thromboembolism (VTE). Active cancer contributes a 4-7 fold increased risk for VTE; however, the incidence of VTE stratified by subpopulations of patients diagnosed with cancer, especially race/ethnicity, is uncertain.
Objective: Describe the incidence of VTE among adult patients (age ≥ 18 years) with a cancer diagnosis in Oklahoma County, OK according to age, gender, race, and cancer type.
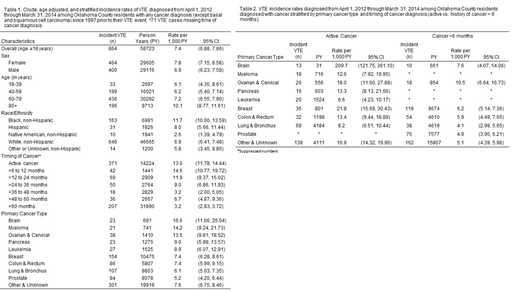
Methods: In collaboration with the Centers for Disease Control and Prevention, we established a population-based surveillance system for VTE in Oklahoma County, OK between April 1, 2012-March 31, 2014 to estimate the incidences of first-time and recurrent VTE events. The Commissioner of Health made VTE a reportable condition and delegated surveillance-related responsibilities to the University of Oklahoma, College of Public Health. Active surveillance involved reviewing imaging studies (e.g., chest computed tomography and compression ultrasounds of the extremities) from all inpatient and outpatient facilities in the county and collecting demographic, treatment and risk factor data on all VTE case-patients. Patients were linked to the Oklahoma Central Cancer Registry. Any patient with a cancer diagnosis since 1997, excluding basal or squamous cell carcinoma, were included in the population-at-risk. Active cancer was defined as metastatic or a diagnosis ≤6 months before their VTE diagnosis. Poisson regression was used to estimate incidence rates (IRs) and 95% confidence intervals (CIs), which are reported per 1,000 person years (PY). Estimates with <10 events were suppressed.
Results: Among all patients aged ≥18 years with a cancer diagnosis since 1997, 1.5% (n = 881) had a VTE event during the 2-year surveillance period. The overall annual age-adjusted incidence of VTE among those with cancer was 6.8 per 1,000 PY (95% CI: 5.81, 7.95). The demographic-specific incidence rates are summarized in Table 1. The VTE incidence did not significantly differ by sex. When stratified by age, annual VTE incidence was similar among those aged 18-39 years (6.1/1,000 PY, 95% CI: 4.35, 8.61), 40-59 years (6.2/1,000 PY, 95% CI: 5.4, 7.14), and 60-79 years (7.2/1,000 PY, 95% CI: 6.55, 7.90), however, the incidence was significantly higher (p<0.05) in those aged 80+ years (10.1/1,000 PY, 95% CI: 8.77, 11.61). When patients with a cancer diagnosis were stratified by race/ethnicity, non-Hispanic blacks had the highest VTE incidence (11.7/1,000 PY, 95% CI: 10.00, 13.59), followed by Hispanics (8.0/1,000 PY, 95% CI: 5.66, 11.44), non-Hispanic whites (6.9/1,000 PY, 95% CI: 6.41, 7.48), other non-Hispanic/unknown (5.8/1,000 PY, 95% CI: 3.45, 9.85), and non-Hispanic Native Americans (2.6/1,000 PY, 95% CI: 1.39, 4.79). VTE incidence was highest among those with active cancer or a history of cancer within the past three years, after which it appeared to decrease. When stratified by primary cancer type, VTE incidence was highest among those with brain cancer (16.6/1,000 PY, 95% CI: 11.06, 25.04) and lowest among those with prostate cancer (5.2/1,000 PY, 95% CI: 4.20, 6.44). As shown in Table 2, when stratified by cancer type, the incidence of VTE was higher (non-overlapping CIs) among those with active cancer compared to those with a history of cancer >6 months for several tumor types.
Discussion: The incidence of VTE among those with cancer differs by race/ethnicity, with non-Hispanic blacks bearing the highest burden of disease. The risk of VTE persists and is particularly elevated up to three years after a cancer diagnosis.
Raskob:Eli Lilly: Consultancy; Pfizer: Consultancy, Honoraria; Portola: Consultancy; Novartis: Consultancy; BMS: Consultancy, Honoraria; Janssen R&D, LLC: Consultancy, Honoraria; Tetherex: Consultancy; Daiichi Sankyo: Consultancy, Honoraria; Anthos: Consultancy; Bayer Healthcare: Consultancy, Honoraria; Boehringer Ingelheim: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal