Introduction: Heparin induced thrombocytopenia (HIT) is a serious prothrombotic condition, usually triggered by exposure to heparin products with formation of antibodies to platelet factor 4/ heparin polyanion complexes. Diagnostic algorithm for HIT combines clinical scoring (4T score) with time sensitive screening for HIT antibodies (HIT-ab), while serotonin release assay (SRA) is remains the gold standard for confirmatory diagnosis. The rate of utilization of 4T score was low in our institution, resulting in inappropriate orders for HIT-Ab test and subsequent administration of unnecessary alternative anticoagulation (AC) in patients with false positive results. In this project, we designed a structured HIT diagnostic workflow incorporating 4T score calculation in our electronic medical record (EMR) and replaced particle immunofiltration assay (PIFA) with latex immunoturbidometric assay (LIA) in our laboratory for HIT-Ab screening, with an aim to improve the rate of 4T utilization and accuracy of HIT diagnosis in a cost-efficient manner.
Methods: In phase I, we performed a retrospective chart review of all patients with PIFA ordered between March 2017-March 2018. Two investigators independently calculated 4T, collected data on results of HIT-Ab, confirmatory SRA tests, and the duration of alternative AC from each record. Any variations in 4T score were resolved by a senior investigator. In phase II, we implemented a new workflow in the EMR incorporating mandatory calculation of 4T score with every order for HIT-Ab test. Our lab started using LIA in place of PIFA. Charts were reviewed on patients with HIT-Ab orders (LIA) from January-June of 2019.
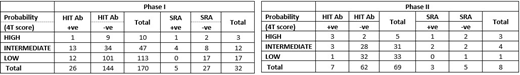
Results: On review of data from phase I, we noted that 4T score was documented in only 5 (0.02%) of 170 patients in whom a PIFA test was ordered. Per investigators assessment, 113 (66.4%) patients had low probability (4T ≤ 3), 47 (27.6%) had intermediate probability (4T 4 or 5), and 10 (5.8%) had a high probability (4T ≥ 6) for a diagnosis of HIT. SRA was ordered in 32 patients, although 17 of them had low probability per investigator assessment. PIFA test came back positive in 26 patients, of whom 16 had corresponding SRA results, and three samples were positive for SRA. PIFA was negative in two patients with confirmed HIT (SRA positive). A total of 19 patients received alternate AC in the first phase, 7 of them had low 4T score per our assessment. In phase II, 69 records were found with available LIA results, showing a relative decrease in HIT-Ab orders compared to earlier phase at the six months mark. Documentation of 4T score has been 100% by ordering physicians, a certain improvement from phase I. Investigator calculated 4T score showed low probability in 33 (47.8%) patients, intermediate probability in 31 (44.9%) patients, high probability in 5 (0.07%) patients. LIA was positive in 7 of the 69 ordered tests, 6 of whom scored high/intermediate in the 4T score. HIT diagnosis was confirmed in 3 of these 7 patients with a positive SRA result. During this period, all the 7 of the eight patients who received alternate AC had a high or intermediate probability for HIT as per 4T.
Conclusion: Our study demonstrated that the successful implementation of a structured protocol for HIT diagnosis ensured 100% adherence to the calculation and documentation of 4T score by clinicians, and significantly reduced the number of inappropriate HIT-Ab test orders in our institution. Use of alternate AC was also more consistent with the level of probability for HIT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal