
Sickle cell Disease (SCD) is the most common inherited blood disorder in the US and is associated with significant morbidity and mortality. Vaso-occlusive crisis (VOC) is a frequent complication of SCD and the most common reason that patients seek medical care. The National Heart and Blood Lung Institute (NHBLI) guidelines recommend supportive care for acute VOC, which includes rapid assessment, hydration, and initiation of analgesic therapy within 60 minutes of registration. After moving to a new location, the Johns Hopkins Sickle Cell Infusion Center (SCIC) was found to have an increase in time to first dose (TTFD). We describe our experience with implementing a new intervention of audit and feedback to decrease our TTFD. As a second objective, we examine whether TTFD of parenteral medication within (≤) 60 minutes of arrival impacts important clinical outcomes of patient-reported pain, acute care utilization, and disposition after a SCIC visit.
Methods: We implemented the audit and feedback intervention in October 2018 at the SCIC. We created a report with the help of the electronic medical record to calculate the TTFD, measured from time of registration to time of first parenteral dose of analgesic medication. TTFD was subdivided into time spent in waiting room, time spent with provider, and time from medication order to administration, allowing us to provide detailed feedback to medical staff involved in these specific processes. This report was generated weekly and results were shared with medical staff and feedback requested. Initial and final pain scores, acute care utilization (acute return visits within 7 days), and SCIC visit disposition were collected. Univariate analysis and logistic regression were performed for TTFD and clinical outcomes.
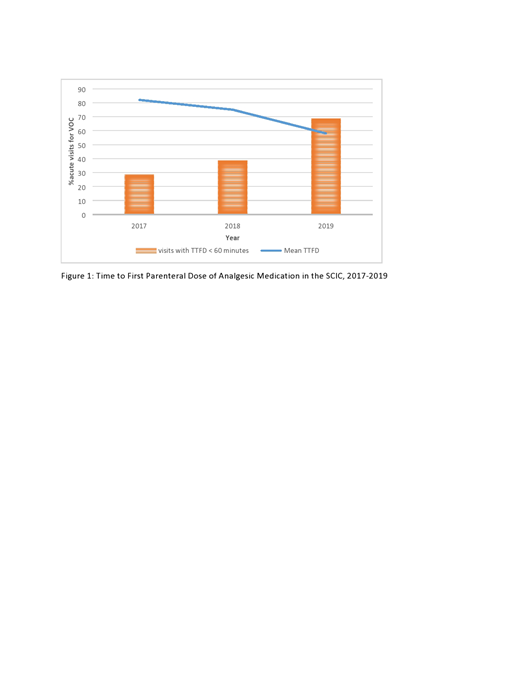
Results: We analyzed data from 1454 unique weekday visits for patient with all SCD genotypes from January 2017 to June 2019, excluding emergency department (ED) transfers. The total number of acute visits for VOC were 647, 570, and 237 respectively for 2017, 2018, and 2019. Of the acute visits, 81.6% were discharged home, 14.1% were transferred to the ED, and 4.0% were admitted. After implementing the audit and feedback method in 2018, we found a significant decrease in the mean TTFD from 75 ± 38 minutes in 2018 to 58 ± 31 minutes in 2019 (Figure 1; p=0.0001). Furthermore, the percentage of acute visits achieving a TTFD ≤ 60 minutes increased annually (28.7%, 38.9%, and 68.7%, respectively). In assessing patient outcomes, for visits with TTFD ≤ 60 minutes the mean discharge pain score was lower (6.05 ± 2.00) than if TTFD was > 60 minutes (6.38 ± 1.93; p = 0.01), despite similar initial reported pain scores and controlling for the visit year. The number of acute return visits within 7 days was lower if TTFD was ≤ 60 minutes compared to > 60 minutes (0.30 ± 0.46 vs 0.37 ± 0.48; p = 0.006), however this difference did not remain statistically significant in multivariate analysis after controlling for year of visit. Surprisingly, the likelihood that a visit would end with patient being discharged home SCIC was higher for those with TTFD > 60 minutes( OR 1.4, CI 1.07-1.88).
Limitations: Our TTFD model did not take into account potential confounders such as nurse to patient ratio, annual clinic policy changes, presence of central vascular access, patient comorbidities, and individual patient utilization behavior.
Conclusion: Audit and feedback was an effective method to reduce the TTFD. Pain at discharge was lower for visits with TTFD ≤ 60 minutes. However, acute care utilization within 7 days of the visit was unchanged based on the TTFD. Further evaluation to better understand patient characteristics that might impact the likelihood of admission after a visit to the SCIC and evaluate the association between longer waits for medication and a decrease in risk of admission is planned.
Lanzkron:Pfizer: Research Funding; Global Blood Therapeutics: Research Funding; Ironwood: Research Funding; HRSA: Research Funding; NIH: Research Funding; PCORI: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal