Background: Many Chinese patients with hematologic disease, who need allogeneic hematopoietic stem cell transplantation(HSCT) commonly lack an HLA matched sibling since a Chinese family often has a single child due to Chinese one-child policy in the past 10years. As an alternative option, unrelated HSCT is the feasible option for the patients without matched related donors (MRD). Many study have found that thalassemia-free survival (TFS) was approximately 90% in unrelated donor HSCT (UDT) for TM patients. Donor selection is one of key factors for better outcomes after hematopoietic stem cell transplantation (HSCT). Choosing the most suitable donors for TM patients can be challenging to physicians and search coordinators. It is shown that increased donor age is associated with high mortality. However, outcomes of donor factors such as age, sex, CMV status, ABO type, matching of HLA loci and female donor pregnancy history for TM patients have rare been taken into account and evaluated.
Aims: The aim of this study was to develop and validate the principal of donor selection and to evaluate the impact of donor characteristics on survival outcomes especially in case of mismatch unrelated donor.
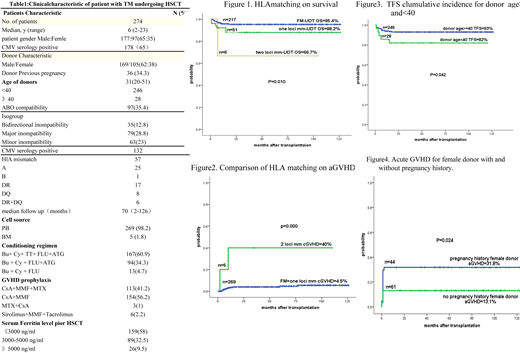
Patients and Methods: Between December 2008 to December 2018,274 TM patients with a median age of 6 years (2-23) had no suitable matched related donor performed an unrelated HSCT. 189 patients have been typed by high resolution (HR) HLA typing for HLA-A/B/C/DRB1 loci, at the start of the donor's search process and 85 typed by high resolution (HR) HLA typing for HLA-A/B/C/DRB1/DQB1 loci. Patients, donors and transplant characteristics are summarized in Table 1
Result: 217 (79.2%) recipient were HLA full matched (FM) with donors, 51 (18.6%) of recipient-donor pairs were HLA one locus mismatched (mm) and 6 (2.2%) two loci mm . Statistically significant differences were observed in overall survival (OS) and thalassemia-free survival (TFS) among full matched group, one loci mm matched group and two loci mm group, the corresponding OS, TFS were 95.4%,88.2%,66.7% (P=0.010,shown in Figure one) and 93%,88%,66.7% (P=0.089) respectively. Risks for cGVHD were higher in recipient-donor HLA-mm transplantation, particularly significant in two loci mm transplant,P=0.000(Figure2).
ABO compatibility did not affect OS and TFS (94.8 vs. 93%,P=0.572 and 94.8% vs. 90.2, P=0.190 respectively in ABO matched group and ABO mismatched group), whereas ABO mismatched was associated with higher rate of graft rejection (GR) although not statistically significant ( 0% vs. 4.3%, P=0.069).
Notably, donor age was significantly associated with worse survival. Both OS and TFS for donor older than 40 years old was significantly worse than those <40 years old(94.6%vs.85% P=0,051)and (93% vs.82%, P=0.042) respectively( Figue3).
Interestingly, previous pregnancy of female donors prior to donation had an impact on acute GVHD, parous female donors resulted in a significantly increased risk of aGVHD (31.8 vs. 13.1%,P=0.024) .
However, donor other characteristics such as sex, parity, and cytomegalovirus serostatus were not associated with survival . For CMV- recipients, a CMV+ donor was not significantly associated with an increase in OS or TFS (92.7 vs. 93.3%, P=0.998, P=0.998 and 90.5% vs. 93.3%;P=0.601 respectively).
Conclusion:Donor age and donor-recipient HLA match are important when selecting unrelated donors. Transplants from donors older than 40 years old should probably be avoided. Younger donors associates with better overall survival and lower rates of acute and cGVHD. When selecting unrelated donors, avoidance of parous female donors if possible as to avoid high incidence of aGVHD. Other donor characteristics such as sex, parity, and cytomegalovirus serostatus were not associated with survival. ABO mismatching (any type: major, minor or bidirectional) was not associated with OS, TFS or GVHD but related to graft rejection. In the future we will observe ABO mismatch among donors and recipients on engraftment time.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal