Background: Post-transplant high dose cyclophosphamide (PT-CY) effectively prevents graft-versus-host disease (GVHD) after unmanipulated HLA-haploidentical hematopoietic stem cell transplantation (HSCT). The use of PT-CY in HLA-identical donor is less explored. In this study, we analyzed the results of PT-CY for GVHD prophylaxis in matched unrelated donor (MUD) HSCT and compared them with those obtained after prophylaxis with anti-thymocyte globulin (ATG), methotrexate (MTX) and cyclosporine (CsA).
Methods: 132 matched unrelated donor HSCT from 4 Spanish centers have been analyzed: 60 performed between 2010 and 2018 using ATG-MTX-CsA and 72 performed between 2014 and 2018 using PT-CY.
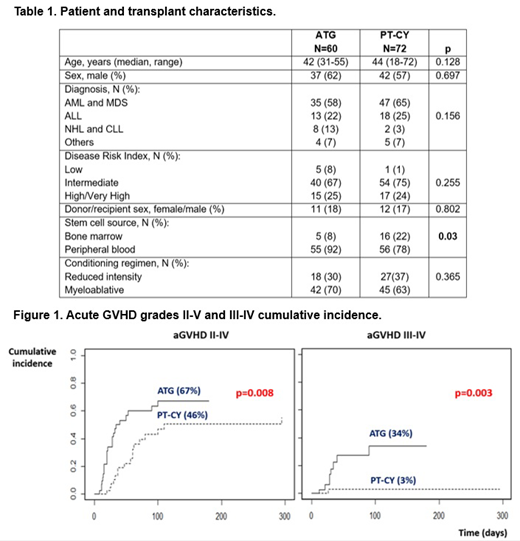
Results: Baseline characteristics and post-transplant complications are shown in Table 1. Peripheral blood was used as graft source in 92% of the patients in the ATG group and in 78% in the PT-CY group. GVHD prophylaxis consisted in rabbit ATG either 2mg/kg days -4 to -2 (41 patients, 68%) or 0.5mg/m2 on day -3 followed by 1mg/kg days -2 and -3 (19 patients, 32%), MTX days +1, +3, +6 and +11, and CsA from day -1 in the ATG group. The PT-CY group received cyclophosphamide 50 mg/kg/d on days +3 and +4, followed by either CsA or tacrolimus plus mycophenolate mofetil (MMF) from day +5 in 30 patients (42%), or cyclophosphamide on days +3 and +5 combined with CsA or tacrolimus in 42 patients (58%; 16 out of them also received sirolimus due to 9/10 HLA-match). Cumulative incidence of grade II-IV (67% vs 46%, p=0.008) and III-IV (34% vs 3%, p=0.003) acute GVHD, were significantly higher in the ATG group (Figure 1). There were no differences in the 2-year cumulative incidence of chronic moderate to severe GVHD (23% vs 24%, p=0.86). After a median follow-up of 78 months for the ATG group and 26 months for the PT-CY group, no differences were found in the 2-year overall survival (58% vs 60%, p=0.475), 2-year event-free survival (51% vs 50%, p=0.961) and the composite endpoint of GVHD-free and relapse-free survival (44% vs 40%, p=0.742). The 2-year cumulative incidence of relapse (22% vs 26%, p=0.67) and non-relapse mortality (NRM) (24% vs 22%, p=0.68) were also similar between both groups. However, NRM in the ATG group was due to GVHD in 9 out of 16 patients, while in the PT-CY group NRM was mostly due to infections and organ toxicity and only 3 out of 15 patients died due to GVHD. The incidence of sinusoidal obstruction syndrome was low in both groups (0% vs 4%, p=0.11). CMV reactivation rates were similar (40% vs 51%, p=0.191). However, both hemorrhagic cystitis and EBV reactivation were higher in the ATG group (56% vs 12%, p=0.00, and 5% vs 0%, p=0.05, respectively).
Conclusions: In our experience, GVHD prophylaxis using PT-CY combined with additional immunosuppression after MUD HSCT, using mostly peripheral blood as graft source, resulted in lower incidence of aGVHD compared to prophylaxis based on ATG-MTX-CsA. Although no impact on non-relapse mortality was observed, GVHD associated mortality was higher in the ATG group as well as cystitis and EBV reactivations. Prospective studies with longer follow-up are needed to confirm these observations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal